Post-Inflammatory Hyperpigmentation and Acne: How Are They Related?

Acne is one of the most common skin problems in humans. The pimples and spots it produces are often uncomfortable and distressing for the sufferer. However, post-inflammatory hyperpigmentation is something that can also cause as much, or more, distress than acne itself.
Although we know that it isn’t the right thing to do, when we have spots we try to deal with them in different ways with the sole objective of making them disappear from the skin.
The problem with doing this is that we make the spot worse. We damage the skin around it even more, spreading the infection to other areas, and we end up making that part of the skin darken.
Acne doesn’t just leave scars. It can also leave “marks” that are quite uncomfortable. Let’s see more about this below.
Causes of hyperpigmentation
As noted in the MSD Manual, hyperpigmentation – also known as hyperpigmentation caused by inflammation or post-inflammatory hyperchromia – “can occur as a result of injuries, such as cuts and burns, or from inflammation caused by conditions such as acne and lupus.”
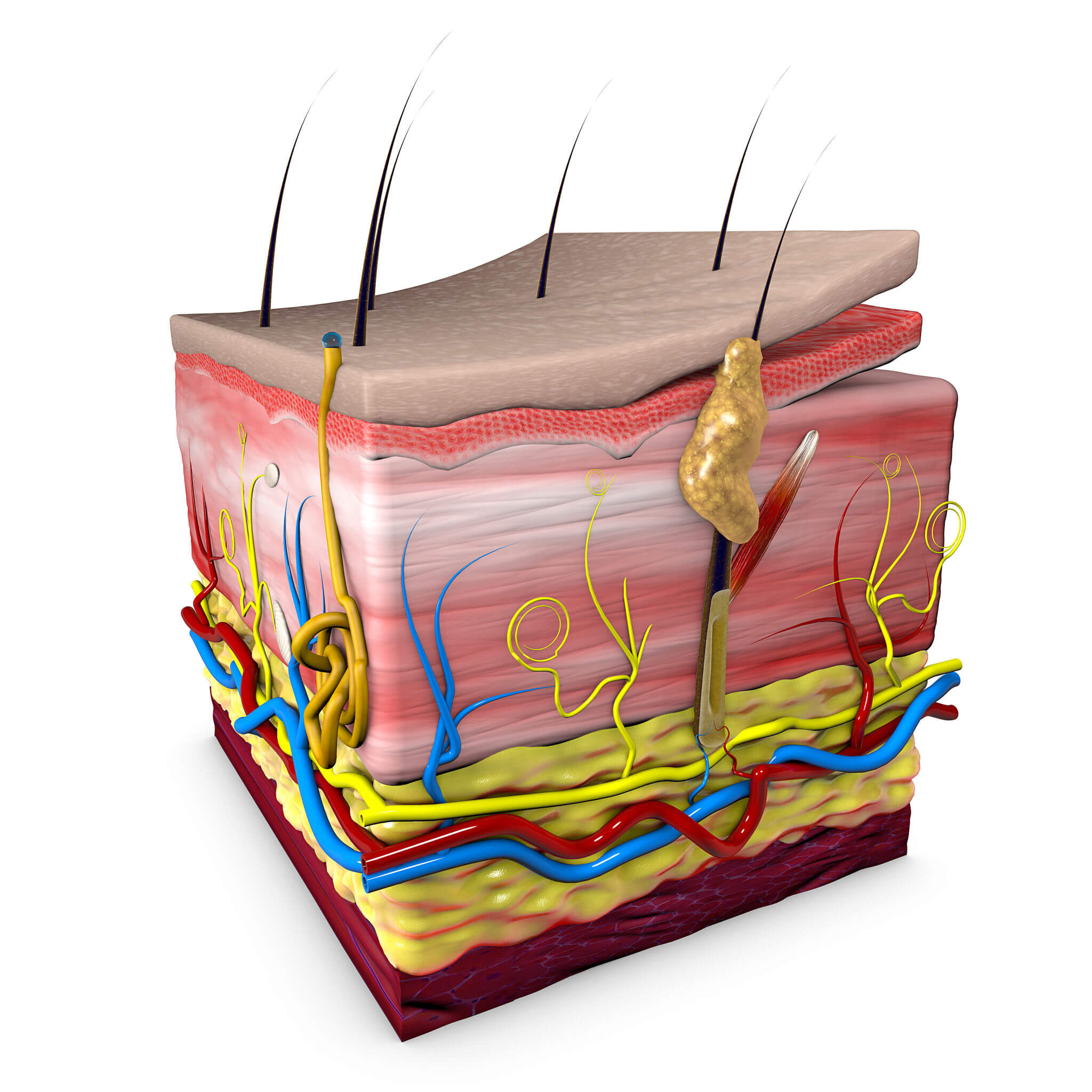
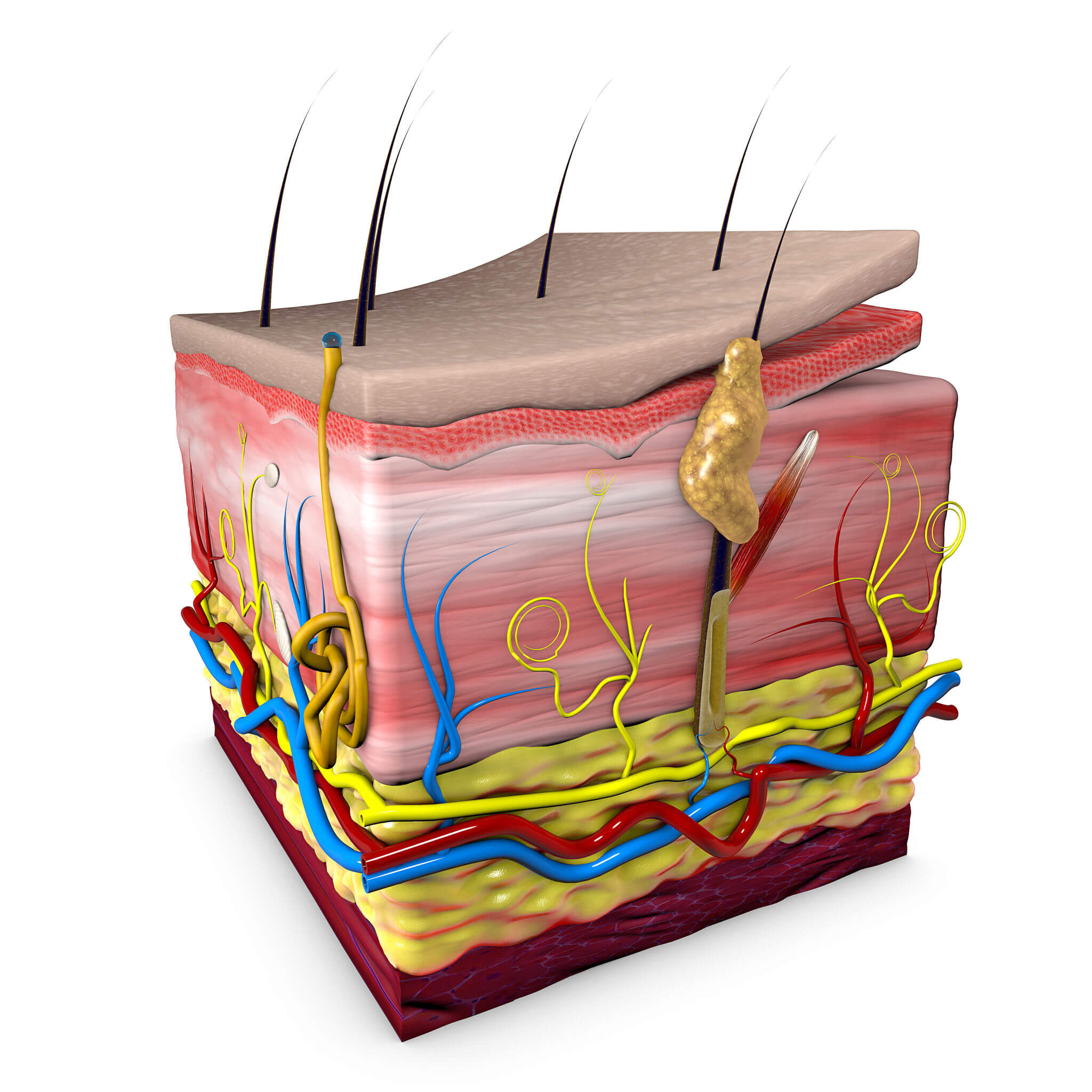
In other words: after injury or inflammation, depending on how you heal, melanocytes produce more melanin. For example, after having handled a quite inflamed spot, after the scab falls off, we’ll notice skin of a different, darker tone in its place.
Symptoms
Post-inflammatory hyperpigmentation can affect both men and women, regardless of their complexion tone.
It’s characterized by producing areas of color different from the rest of the complexion. These are dark areas or marks that can vary according to the person’s skin tone and how much skin is involved.
- The markings can be pinkish, reddish, purple, brown, or even black.
- In the case of acne, although it’s common for marks to be the result of handling the spots, they can also appear as a result of some skin treatments, such as dermabrasion and chemical peels. For this reason, in many cases, consultation with the dermatologist is vital.
- People with a medium to dark complexion tend to have more severe and long-lasting marks, as indicated by scientific evidence.
- Many people with acne (or who have had acne at some point in their life) have some degree of post-inflammatory hyperpigmentation.
The time factor
In many cases of post-inflammatory acne hyperpigmentation, the marks fade over time. But for this to happen without a trace, the ideal is to limit prolonged exposure to the sun, and be patient.
As indicated in an article published in Elsevier magazine, it’s recommended that people with hyperpigmentation use a sunscreen daily, according to their skin type, all year round, even on cloudy days. Mainly to prevent a greater darkening of the affected areas, as well as a greater disparity in the tone of the skin in general.
The authors of the article also indicate that, although treatment for post-inflammatory hyperpigmentation isn’t always necessary, there are several options. We’ll talk about them below.
Treatment

In addition to protecting the skin from the sun and evaluating the skin’s healing progress over time, in some cases it may be necessary to apply a depigmenting treatment. On this, the aforementioned article states the following:
- Hydroquinone is a very common depigmenting substance in post-inflammatory hyperpigmentation treatments. It can be found in concentrations of 2 to 10%. Although only from 2% onwards a medical prescription is required.
- Depending on the type of skin, the dermatologist may consider one concentration or another. All this to prevent annoying reactions, such as irritation, redness and peeling.
- Hydroquinone treatment is often indicated if it’s a prolonged treatment. From 2 to 3 months onwards.
- Kojic acid is very helpful in treating post-inflammatory hyperpigmentation. It’s usually combined with glycolic acid or hydroquinone, but, unlike the latter, its irritating effects are much milder.
- There are depigmenting formulas that have a certain sun protection factor included, but even so, its effectiveness is reduced. However, it’s recommended to apply a high factor sunscreen, in addition.
- Whatever the product, it should never be applied to open wounds, burns, mucous membranes or areas with eczema.
- If the marks don’t improve after two months of treatment, it’ll be essential to consult a dermatologist.
- Chemical peels and laser therapy are also treatment options in cases where the skin doesn’t respond to topical medications.
What to do about it?
If you notice that, after suffering an injury, your skin is prone to pigmentation, we would recommend that you consult with your dermatologist about the type of products you should use daily, as well as the measures that would be most appropriate for your case. The prevention of hyperpigmentation plays as important a role as adherence to the treatment itself.
If you suffer from psoriasis, atopic dermatitis, acne, or have burned skin, you should also consult with the specialist as to what you should do to take care of yourself and prevent adverse reactions.
Unfortunately, it isn’t a good idea to use any over-the-counter products with lightening properties, as they could make the problem worse rather than improve it. For this reason, it’s better to hear an expert’s opinion and proceed confidently with what they recommend.
Acne is one of the most common skin problems in humans. The pimples and spots it produces are often uncomfortable and distressing for the sufferer. However, post-inflammatory hyperpigmentation is something that can also cause as much, or more, distress than acne itself.
Although we know that it isn’t the right thing to do, when we have spots we try to deal with them in different ways with the sole objective of making them disappear from the skin.
The problem with doing this is that we make the spot worse. We damage the skin around it even more, spreading the infection to other areas, and we end up making that part of the skin darken.
Acne doesn’t just leave scars. It can also leave “marks” that are quite uncomfortable. Let’s see more about this below.
Causes of hyperpigmentation
As noted in the MSD Manual, hyperpigmentation – also known as hyperpigmentation caused by inflammation or post-inflammatory hyperchromia – “can occur as a result of injuries, such as cuts and burns, or from inflammation caused by conditions such as acne and lupus.”
In other words: after injury or inflammation, depending on how you heal, melanocytes produce more melanin. For example, after having handled a quite inflamed spot, after the scab falls off, we’ll notice skin of a different, darker tone in its place.
Symptoms
Post-inflammatory hyperpigmentation can affect both men and women, regardless of their complexion tone.
It’s characterized by producing areas of color different from the rest of the complexion. These are dark areas or marks that can vary according to the person’s skin tone and how much skin is involved.
- The markings can be pinkish, reddish, purple, brown, or even black.
- In the case of acne, although it’s common for marks to be the result of handling the spots, they can also appear as a result of some skin treatments, such as dermabrasion and chemical peels. For this reason, in many cases, consultation with the dermatologist is vital.
- People with a medium to dark complexion tend to have more severe and long-lasting marks, as indicated by scientific evidence.
- Many people with acne (or who have had acne at some point in their life) have some degree of post-inflammatory hyperpigmentation.
The time factor
In many cases of post-inflammatory acne hyperpigmentation, the marks fade over time. But for this to happen without a trace, the ideal is to limit prolonged exposure to the sun, and be patient.
As indicated in an article published in Elsevier magazine, it’s recommended that people with hyperpigmentation use a sunscreen daily, according to their skin type, all year round, even on cloudy days. Mainly to prevent a greater darkening of the affected areas, as well as a greater disparity in the tone of the skin in general.
The authors of the article also indicate that, although treatment for post-inflammatory hyperpigmentation isn’t always necessary, there are several options. We’ll talk about them below.
Treatment

In addition to protecting the skin from the sun and evaluating the skin’s healing progress over time, in some cases it may be necessary to apply a depigmenting treatment. On this, the aforementioned article states the following:
- Hydroquinone is a very common depigmenting substance in post-inflammatory hyperpigmentation treatments. It can be found in concentrations of 2 to 10%. Although only from 2% onwards a medical prescription is required.
- Depending on the type of skin, the dermatologist may consider one concentration or another. All this to prevent annoying reactions, such as irritation, redness and peeling.
- Hydroquinone treatment is often indicated if it’s a prolonged treatment. From 2 to 3 months onwards.
- Kojic acid is very helpful in treating post-inflammatory hyperpigmentation. It’s usually combined with glycolic acid or hydroquinone, but, unlike the latter, its irritating effects are much milder.
- There are depigmenting formulas that have a certain sun protection factor included, but even so, its effectiveness is reduced. However, it’s recommended to apply a high factor sunscreen, in addition.
- Whatever the product, it should never be applied to open wounds, burns, mucous membranes or areas with eczema.
- If the marks don’t improve after two months of treatment, it’ll be essential to consult a dermatologist.
- Chemical peels and laser therapy are also treatment options in cases where the skin doesn’t respond to topical medications.
What to do about it?
If you notice that, after suffering an injury, your skin is prone to pigmentation, we would recommend that you consult with your dermatologist about the type of products you should use daily, as well as the measures that would be most appropriate for your case. The prevention of hyperpigmentation plays as important a role as adherence to the treatment itself.
If you suffer from psoriasis, atopic dermatitis, acne, or have burned skin, you should also consult with the specialist as to what you should do to take care of yourself and prevent adverse reactions.
Unfortunately, it isn’t a good idea to use any over-the-counter products with lightening properties, as they could make the problem worse rather than improve it. For this reason, it’s better to hear an expert’s opinion and proceed confidently with what they recommend.
- Benavides, Nereyda González, Juan Carlos Robles Méndez, and Jorge Ocampo Candiani. 2018. “Artículo de Revisión: Hiperpigmentaciones Adquiridas Acquired Hyperpigmentations: A Review.”
-
Daas, S. 2019. “Hiperpigmentación.” Manual MSD Versión Para Profesionales. 2019. https://www.msdmanuals.com/es/professional/trastornos-dermatológicos/trastornos-de-la-pigmentación/hiperpigmentación.
- Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010 Jul;3(7):20-31. PMID: 20725554; PMCID: PMC2921758.
-
“Hiperpigmentación | Farmacia Profesional.” n.d. Accessed June 2, 2021. https://www.elsevier.es/es-revista-farmacia-profesional-3-articulo-hiperpigmentacion-13092625.
-
Keri, Jonette E. n.d. “Acné – Trastornos de La Piel – Manual MSD Versión Para Público General.” Manual MSD- Versión Para Público General. Accessed June 1, 2021. https://www.msdmanuals.com/es/hogar/trastornos-de-la-piel/acné-y-trastornos-relacionados/acné.
-
Saeedi, Majid, Masoumeh Eslamifar, and Khadijeh Khezri. 2019. “Kojic Acid Applications in Cosmetic and Pharmaceutical Preparations.” Biomedicine and Pharmacotherapy. Elsevier Masson SAS. https://doi.org/10.1016/j.biopha.2018.12.006.
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.







