What Is Dermoscopy?

Skin lesions are a common reason for consultation at the health center or hospital. The dermatology specialist usually uses various tools that help to identify skin conditions. Are you interested in knowing what dermoscopy is? Keep reading and we’ll tell you.
Dermoscopy or surface microscopy is a very useful method in the diagnosis of lesions suggestive of skin cancer. It allows a detailed assessment of the skin surface in real time and without causing discomfort to the patient.
This has multiple applications, making it one of the main techniques used by dermatologists around the world.
What is dermoscopy?
Currently, dermoscopy is a clinical diagnostic tool performed with the help of a small device called a dermatoscope. It’s made up of a specialized magnifying lens system and a direct light source that allows it to amplify and analyze the skin characteristics.
Studies affirm that the dermatoscope makes it possible to make the stratum corneum of the skin translucent. This favors the visualization of the structures contained in the epidermis that aren’t visible to the naked eye. Skin lesions are evaluated based on their shape, color, texture, symmetry, diameter, and borders.
Dermoscopy can be performed with two types of dermatoscopes, with an immersion and contact device as well as one that uses polarized light with different magnifying filters. However, they follow the same concept of lighting and amplification of everything present on the skin.
Why is dermoscopy done?
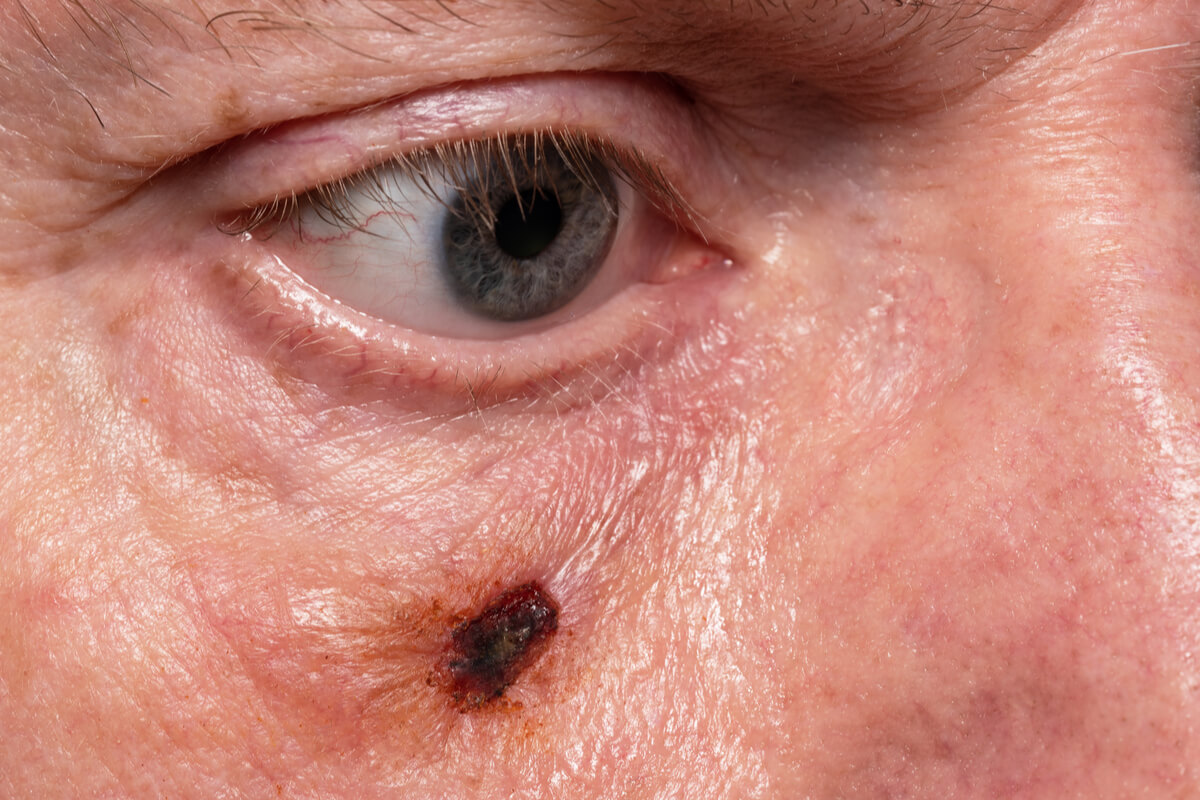
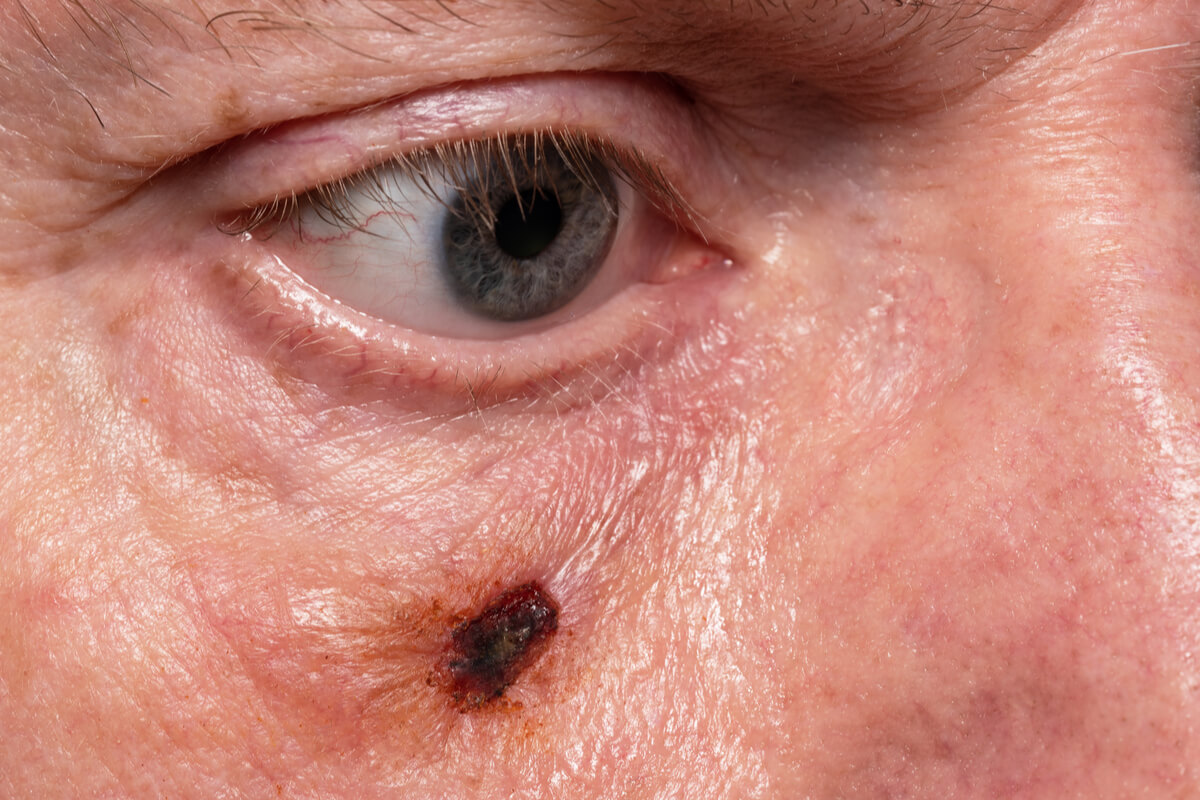
In general, the specialist doctor decides to perform this procedure when they see a spot, mole or plaque with abnormal signs on the skin. This is part of the comprehensive physical examination in the dermatology units. Some research suggests that it’s widely useful in the early diagnosis of melanoma and basal cell cancer.
Similarly, it’s used in the differential diagnosis of cancerous and non-cancerous skin lesions. In this sense, it’s used in the identification of other skin conditions such as actinic keratosis, hemangiomas, nevi or moles, psoriasis, lichen planus, dermatofibroma, and benign lentigo.
Dermoscopy is considered the first step before recommending a biopsy or the removal of a mole suspected of cancer. In this way, an unnecessary invasive procedure is avoided. In addition, studies show that it allows early identification and treatment of vitiligo.
Risks and contraindications
These days, this diagnostic method is considered very safe throughout the world. It’s useful for any skin type or age group. Dermoscopy is a simple, non-invasive and painless technique, and so it’s not associated with risks of infection or traumatic injuries.
What to expect during dermoscopy?
To start the procedure, the doctor will apply a gel or oil-based solution to the skin region to be evaluated. This substance acts as an immersion liquid, allowing a clearer and more detailed image of the skin to be obtained.
Once the gel has been applied, the specialist will bring the dermatoscope closer and into contact with the skin. It will apply a slight pressure with the equipment on the surface, which doesn’t usually produce any kind of discomfort. This is done in order to eliminate or reduce any air bubbles present in the gel that may interfere with visualization.
In this way, an amplified image of the tissue or lesion to be studied can be obtained. In some cases, the dermatologist may move the device closer or farther to obtain a sharper field. In general, the dermatoscope allows images or videos of the procedure to be captured and stored, which favors long-term monitoring and control of lesions.
On the other hand, in the dermatoscope with polarized light, no contact is generated between the equipment lenses and the patient’s skin. The technique is similar to that performed with conventional equipment, however, in this method, the device is kept at a distance of about 1 centimeter from the skin surface.
Interpretation of results

Dermoscopy is a real-time procedure, so the results are obtained immediately. This study offers important data about the lesions present on the skin, which will be analyzed by the specialist to make a presumptive diagnosis.
In this sense, the information about the pigmentation and real distribution of the tissue lesions is evaluated. In addition, the pattern of the blood vessels is evaluated and other conditions that can’t be seen with the naked eye are located.
The shades observed during the study depend on the source of the pigment, such as melanin or hemoglobin, and the layer of skin where the skin lesion is located. The isolated study of the coloration is not useful in the identification of skin cancer, however, in melanoma it allows the detection of atypical cell proliferations.
If a cutaneous neoplasm is suspected, the specialist may indicate a biopsy to establish a definitive diagnosis and initiate the approach to the pathology.
On the other hand, the dermatologist may recommend monitoring the lesion without the need for immediate removal. Periodic monitoring in subsequent consultations will allow you to confirm or rule out the presence of skin cancer.
If you have any questions, consult your doctor
Dermoscopy is a simple and painless study, which serves as a diagnostic support for the treating physician. It doesn’t require rigorous preparation and can be performed during a routine dermatological consultation. If during the physical examination the specialist considers it necessary, then don’t hesitate to ask any questions you need to in order to clear up any doubts.
Skin lesions are a common reason for consultation at the health center or hospital. The dermatology specialist usually uses various tools that help to identify skin conditions. Are you interested in knowing what dermoscopy is? Keep reading and we’ll tell you.
Dermoscopy or surface microscopy is a very useful method in the diagnosis of lesions suggestive of skin cancer. It allows a detailed assessment of the skin surface in real time and without causing discomfort to the patient.
This has multiple applications, making it one of the main techniques used by dermatologists around the world.
What is dermoscopy?
Currently, dermoscopy is a clinical diagnostic tool performed with the help of a small device called a dermatoscope. It’s made up of a specialized magnifying lens system and a direct light source that allows it to amplify and analyze the skin characteristics.
Studies affirm that the dermatoscope makes it possible to make the stratum corneum of the skin translucent. This favors the visualization of the structures contained in the epidermis that aren’t visible to the naked eye. Skin lesions are evaluated based on their shape, color, texture, symmetry, diameter, and borders.
Dermoscopy can be performed with two types of dermatoscopes, with an immersion and contact device as well as one that uses polarized light with different magnifying filters. However, they follow the same concept of lighting and amplification of everything present on the skin.
Why is dermoscopy done?
In general, the specialist doctor decides to perform this procedure when they see a spot, mole or plaque with abnormal signs on the skin. This is part of the comprehensive physical examination in the dermatology units. Some research suggests that it’s widely useful in the early diagnosis of melanoma and basal cell cancer.
Similarly, it’s used in the differential diagnosis of cancerous and non-cancerous skin lesions. In this sense, it’s used in the identification of other skin conditions such as actinic keratosis, hemangiomas, nevi or moles, psoriasis, lichen planus, dermatofibroma, and benign lentigo.
Dermoscopy is considered the first step before recommending a biopsy or the removal of a mole suspected of cancer. In this way, an unnecessary invasive procedure is avoided. In addition, studies show that it allows early identification and treatment of vitiligo.
Risks and contraindications
These days, this diagnostic method is considered very safe throughout the world. It’s useful for any skin type or age group. Dermoscopy is a simple, non-invasive and painless technique, and so it’s not associated with risks of infection or traumatic injuries.
What to expect during dermoscopy?
To start the procedure, the doctor will apply a gel or oil-based solution to the skin region to be evaluated. This substance acts as an immersion liquid, allowing a clearer and more detailed image of the skin to be obtained.
Once the gel has been applied, the specialist will bring the dermatoscope closer and into contact with the skin. It will apply a slight pressure with the equipment on the surface, which doesn’t usually produce any kind of discomfort. This is done in order to eliminate or reduce any air bubbles present in the gel that may interfere with visualization.
In this way, an amplified image of the tissue or lesion to be studied can be obtained. In some cases, the dermatologist may move the device closer or farther to obtain a sharper field. In general, the dermatoscope allows images or videos of the procedure to be captured and stored, which favors long-term monitoring and control of lesions.
On the other hand, in the dermatoscope with polarized light, no contact is generated between the equipment lenses and the patient’s skin. The technique is similar to that performed with conventional equipment, however, in this method, the device is kept at a distance of about 1 centimeter from the skin surface.
Interpretation of results

Dermoscopy is a real-time procedure, so the results are obtained immediately. This study offers important data about the lesions present on the skin, which will be analyzed by the specialist to make a presumptive diagnosis.
In this sense, the information about the pigmentation and real distribution of the tissue lesions is evaluated. In addition, the pattern of the blood vessels is evaluated and other conditions that can’t be seen with the naked eye are located.
The shades observed during the study depend on the source of the pigment, such as melanin or hemoglobin, and the layer of skin where the skin lesion is located. The isolated study of the coloration is not useful in the identification of skin cancer, however, in melanoma it allows the detection of atypical cell proliferations.
If a cutaneous neoplasm is suspected, the specialist may indicate a biopsy to establish a definitive diagnosis and initiate the approach to the pathology.
On the other hand, the dermatologist may recommend monitoring the lesion without the need for immediate removal. Periodic monitoring in subsequent consultations will allow you to confirm or rule out the presence of skin cancer.
If you have any questions, consult your doctor
Dermoscopy is a simple and painless study, which serves as a diagnostic support for the treating physician. It doesn’t require rigorous preparation and can be performed during a routine dermatological consultation. If during the physical examination the specialist considers it necessary, then don’t hesitate to ask any questions you need to in order to clear up any doubts.
- Kumar Jha A, Sonthalia S, Lallas A, Chaudhary R. Dermoscopy in vitiligo: diagnosis and beyond. International Journal of Dermatology. 2017;57(1):50-54.
- Rodríguez-Cabral R, Montoya-Sosa G, Roldán-Marín R, Carlos-Ortega B. Principios básicos de dermatoscopia. Dermatología Rev Mex 2014;58:300-304.
- Palacios-Martínez D, Díaz-Alonso R. Dermatoscopia para principiantes ( i ): características generales. SEMERGEN – Medicina de Familia. 2017;43(3):216-221.
- Micali G, Lacarrubba F. Dermatoscopy: Instrumental Update. Dermatol Clin. 2018;36(4):345-348.
- Weber P, Tschandl P, Sinz C, Kittler H. Dermatoscopy of Neoplastic Skin Lesions: Recent Advances, Updates, and Revisions. Curr Treat Options Oncol. 2018;19(11):56.
- Brancaccio G, Russo T, Lallas A, Moscarella E, Agozzino M, Argenziano G. Melanoma: clinical and dermoscopic diagnosis. G Ital Dermatol Venereol. 2017;152(3):213-223.
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.







