Vulvovaginal Candidiasis: Symptoms, Causes, and Treatments

Much of the female reproductive system has a perfectly balanced microbiota that protects it from pathogens. However, when this balance is disturbed, the vagina’s own microorganisms can cause infections, one of the most common being vulvovaginal candidiasis.
This is an infectious disease produced by a fungus of the genus Candida, specifically by Candida albicans. This fungus is found in small numbers on the skin, in the mouth, in the gastrointestinal tract, and in the vagina. However, various factors can make it proliferate, thus generating the disease.
Vulvovaginal candidiasis is one of the most frequent vaginal infections. It’s estimated to affect between 70% and 75% of women of childbearing age. Despite everything, there are no representative studies, as it’s often misdiagnosed.
The causes of vulvovaginal candidiasis
Under normal conditions, the vagina has various fungi and bacteria that make up the vaginal flora; including Candida albicans. All these microorganisms are in perfect balance thanks to the acidic pH of the vagina, which prevents their multiplication.
However, these fungi and bacteria are capable of causing an infection when they reproduce excessively or when they penetrate the deeper cell layers. This occurs if the vaginal pH is altered and its acidity decreases, providing the ideal environment for microorganisms to multiply.
In this regard, among the various factors that can influence the excessive growth of fungi and subsequent vulvovaginal candidiasis are the following:
- Medications: The use of oral antibiotics to treat other infections.
- Hormonal changes: Due to pregnancy or an increase in estrogen levels.
- Diseases: Especially uncontrolled diabetes mellitus.
- Impaired immune system or with states of immunosuppression.
- Inadequate vaginal hygiene: This is associated with the constant use of vaginal douches.
It’s important to note that this isn’t considered a sexually transmitted infection, as a woman can suffer from it without having sex. However, some men may develop mild symptoms after having sex with an infected partner and, in turn, pass the infection on to another person.
Symptoms
Vulvovaginal candidiasis will cause vaginitis, that is, inflammation of the vagina, so symptoms can be seen both inside and outside of it. Among the main signs are the following:
- Pruritus: Intense itching and vaginal irritation
- Burning sensation and redness of the area
- Pain: With discomfort when urinating or during sexual intercourse
- Vaginal rash
One of the most characteristic symptoms and one that’s worth highlighting among others is the alteration in vaginal discharge. It will be abundant, thick, and white when you have the infection. However, it won’t have any type of odor, which will allow us to differentiate it from other diseases such as trichomoniasis.
Diagnosis of vulvovaginal candidiasis
Many vaginal problems can appear with a clinic similar to that presented by vulvovaginal candidiasis. In most cases, the doctor will perform a visual inspection in search of white fluid and various whitish plaques on the vaginal walls, although these may not be present.
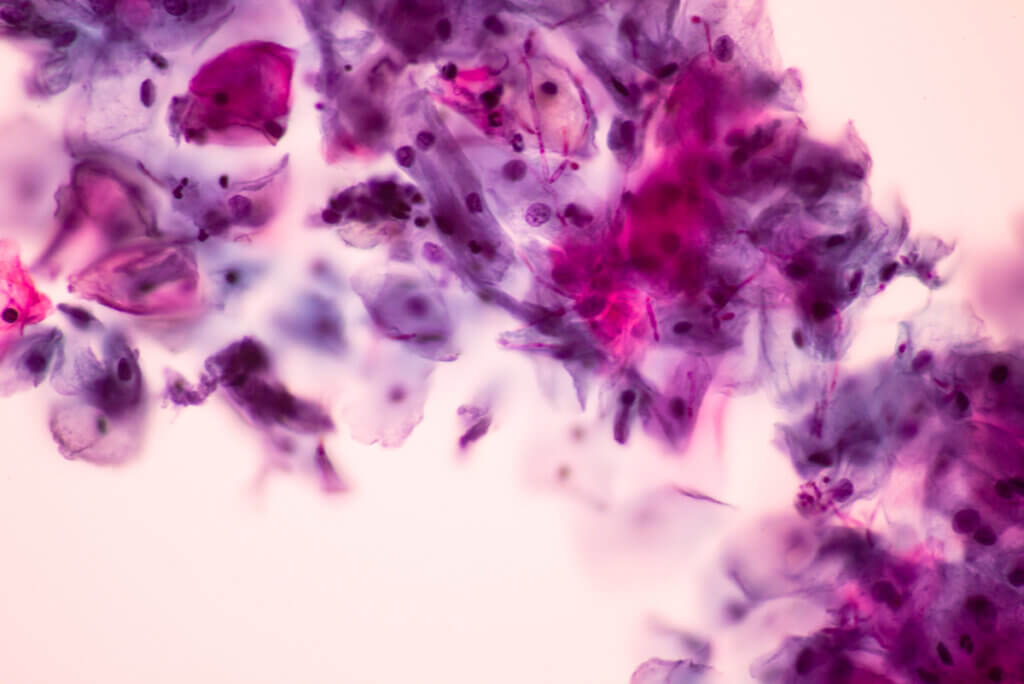
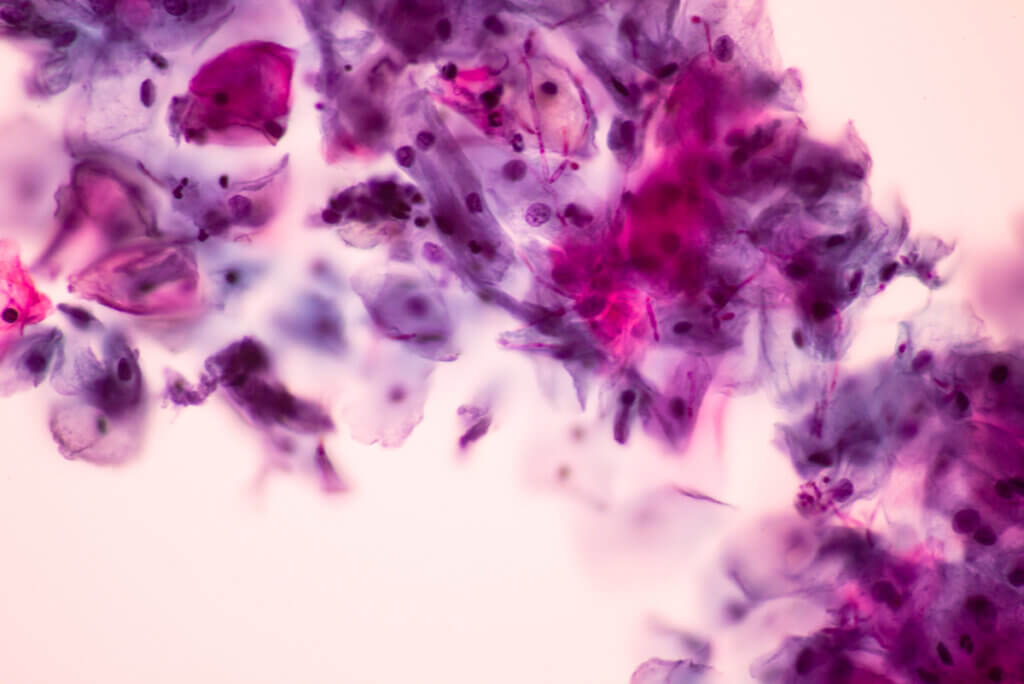
The professional must also take a sample of the vaginal discharge to search for the yeasts of the fungus. In this regard, they may perform a direct observation under the microscope or a Papanicolaou test. Diagnosis also includes a culture to confirm the existence of a mixed infection.
Possible treatments
The treatment of this disease will be aimed at eliminating the fungus and restoring the usual vaginal microbiota. In this regard, candidiasis will be treated with an antifungal, which can be administered vaginally or orally, depending on the severity of the infection.
When the approach is vaginal, clotrimazole cream and ovules are usually applied. On the other hand, in an oral treatment, both fluconazole and itraconazole can be indicated. However, great care must be taken, as both have liver damage among their adverse effects. Sometimes the adjuvant use of probiotics is recommended in order to restore the normal flora.
The duration of treatment will depend on the severity of the infection. It can range from a single application to the administration of medication for 15 days.

Natural remedies against infection
Over the years, various strains of this fungus resistant to fluconazole have emerged, forcing specialists to seek alternative treatments. In this regard, various studies have shown the efficacy of garlic.
In a 2015 study, garlic tablets were shown to reduce symptoms of vulvovaginal candidiasis in 44% of cases in just 7 days. At the same time, it also decreases the SIR2 virulence gene of Candida albicans, thus helping to prevent its proliferation.
Finally, garlic oil in concentrations of 0.35 μg/ml is also capable of penetrating the yeast cell membrane and causing its death. However, more studies are still necessary and it’s important to consult a doctor before starting an alternative therapy.
Hygiene and prevention measures for vulvovaginal candidiasis
Despite being one of the most common vaginal infections, there are various measures that women can take to prevent it. All of them are focused on maintaining adequate intimate hygiene. One of the most important is to clean the genital and anal area from front to back, which will avoid transferring new pathogens to the vagina.
In addition, you should also avoid tight clothing and change used tampons or pads regularly. With these simple but effective measures, it’s possible to greatly reduce the possibility of suffering from vulvovaginal candidiasis and other associated infections.
Much of the female reproductive system has a perfectly balanced microbiota that protects it from pathogens. However, when this balance is disturbed, the vagina’s own microorganisms can cause infections, one of the most common being vulvovaginal candidiasis.
This is an infectious disease produced by a fungus of the genus Candida, specifically by Candida albicans. This fungus is found in small numbers on the skin, in the mouth, in the gastrointestinal tract, and in the vagina. However, various factors can make it proliferate, thus generating the disease.
Vulvovaginal candidiasis is one of the most frequent vaginal infections. It’s estimated to affect between 70% and 75% of women of childbearing age. Despite everything, there are no representative studies, as it’s often misdiagnosed.
The causes of vulvovaginal candidiasis
Under normal conditions, the vagina has various fungi and bacteria that make up the vaginal flora; including Candida albicans. All these microorganisms are in perfect balance thanks to the acidic pH of the vagina, which prevents their multiplication.
However, these fungi and bacteria are capable of causing an infection when they reproduce excessively or when they penetrate the deeper cell layers. This occurs if the vaginal pH is altered and its acidity decreases, providing the ideal environment for microorganisms to multiply.
In this regard, among the various factors that can influence the excessive growth of fungi and subsequent vulvovaginal candidiasis are the following:
- Medications: The use of oral antibiotics to treat other infections.
- Hormonal changes: Due to pregnancy or an increase in estrogen levels.
- Diseases: Especially uncontrolled diabetes mellitus.
- Impaired immune system or with states of immunosuppression.
- Inadequate vaginal hygiene: This is associated with the constant use of vaginal douches.
It’s important to note that this isn’t considered a sexually transmitted infection, as a woman can suffer from it without having sex. However, some men may develop mild symptoms after having sex with an infected partner and, in turn, pass the infection on to another person.
Symptoms
Vulvovaginal candidiasis will cause vaginitis, that is, inflammation of the vagina, so symptoms can be seen both inside and outside of it. Among the main signs are the following:
- Pruritus: Intense itching and vaginal irritation
- Burning sensation and redness of the area
- Pain: With discomfort when urinating or during sexual intercourse
- Vaginal rash
One of the most characteristic symptoms and one that’s worth highlighting among others is the alteration in vaginal discharge. It will be abundant, thick, and white when you have the infection. However, it won’t have any type of odor, which will allow us to differentiate it from other diseases such as trichomoniasis.
Diagnosis of vulvovaginal candidiasis
Many vaginal problems can appear with a clinic similar to that presented by vulvovaginal candidiasis. In most cases, the doctor will perform a visual inspection in search of white fluid and various whitish plaques on the vaginal walls, although these may not be present.
The professional must also take a sample of the vaginal discharge to search for the yeasts of the fungus. In this regard, they may perform a direct observation under the microscope or a Papanicolaou test. Diagnosis also includes a culture to confirm the existence of a mixed infection.
Possible treatments
The treatment of this disease will be aimed at eliminating the fungus and restoring the usual vaginal microbiota. In this regard, candidiasis will be treated with an antifungal, which can be administered vaginally or orally, depending on the severity of the infection.
When the approach is vaginal, clotrimazole cream and ovules are usually applied. On the other hand, in an oral treatment, both fluconazole and itraconazole can be indicated. However, great care must be taken, as both have liver damage among their adverse effects. Sometimes the adjuvant use of probiotics is recommended in order to restore the normal flora.
The duration of treatment will depend on the severity of the infection. It can range from a single application to the administration of medication for 15 days.

Natural remedies against infection
Over the years, various strains of this fungus resistant to fluconazole have emerged, forcing specialists to seek alternative treatments. In this regard, various studies have shown the efficacy of garlic.
In a 2015 study, garlic tablets were shown to reduce symptoms of vulvovaginal candidiasis in 44% of cases in just 7 days. At the same time, it also decreases the SIR2 virulence gene of Candida albicans, thus helping to prevent its proliferation.
Finally, garlic oil in concentrations of 0.35 μg/ml is also capable of penetrating the yeast cell membrane and causing its death. However, more studies are still necessary and it’s important to consult a doctor before starting an alternative therapy.
Hygiene and prevention measures for vulvovaginal candidiasis
Despite being one of the most common vaginal infections, there are various measures that women can take to prevent it. All of them are focused on maintaining adequate intimate hygiene. One of the most important is to clean the genital and anal area from front to back, which will avoid transferring new pathogens to the vagina.
In addition, you should also avoid tight clothing and change used tampons or pads regularly. With these simple but effective measures, it’s possible to greatly reduce the possibility of suffering from vulvovaginal candidiasis and other associated infections.
- Tapia P Cecilia. Candidiasis vulvovaginal. Revista Chilena de Infectología. 2008;25(4):312-312.
- Spence D. Candidiasis (vulvovaginal). BMJ Clinical Evidence. 2010, 0815. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907618/.
- Miró, María Soledad, et al. “Candidiasis vulvovaginal: una antigua enfermedad con nuevos desafíos.” Revista Iberoamericana de Micología 34.2 (2017): 65-71.
- Varadarajan, Saranya, et al. “Invitro anti-mycotic activity of hydro alcoholic extracts of some indian medicinal plants against fluconazole resistant Candida albicans.” Journal of clinical and diagnostic research: JCDR 9.8 (2015): ZC07.
- White DJ, Vanthuyne A. Vulvovaginal candidiasis. Sexually Transmitted Infections. 2006;82:iv28-iv30.
- Barrenetxea Ziarrusta G. Vulvovaginitis candidiásica. Revista Iberoamericana de Micología. 2002;19:22-24.
- Ciudad-Reynaud A. Infecciones vaginales por cándida: diagnóstico y tratamiento. Revista Peruana de Ginecología y Obstetricia. 2007;53:159-166.
- Rivero, M., J. Diaz, and S. Centeno. “Frecuencia de especies de Candida aisladas en pacientes embarazadas con vulvovaginitis.” Revista de la Sociedad Venezolana de Microbiología 23.2 (2003): 148-152.
- Martínez-Pizarro S. Ajo para el tratamiento de la candidiasis vaginal. Revista Chilena de Obsteticia y Ginecología. 2020;85( 4):310-311.
- Alemán Mondeja, Linet Diana, Caridad Almanza Martínez, and Octavio Fernández Limia. “Diagnóstico y prevalencia de infecciones vaginales.” Revista cubana de Obstetricia y Ginecología 36.2 (2010): 62-103.
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.







