The 4 Most Common Gum Diseases


Escrito y verificado por la odontóloga Vanesa Evangelina Buffa
The most frequent gum diseases can put the permanence of the teeth in the mouth at risk. Other conditions compromise the aesthetics of the smile and cause discomfort and pain.
Gingival tissue has the function of protecting and supporting the teeth. Knowing the diseases that affect the gums will allow you to prevent them and take care of this area of the mouth.
Several pathological processes can develop in the gingival tissue. Today, we’ll tell you about the 4 most frequent gum diseases and how to avoid them.
What are the gums and how do the most common gum diseases occur?
The gums are the oral mucosa that surrounds each of the teeth in the mouth, covering the bone that supports them. They function as a protective barrier that prevents bacteria or foreign substances from entering the root area.
Gingival tissue helps teeth remain firm and fixed in the jaws. In addition, it acts as a buffer against the forces that are generated in the mouth, preventing its impact on the underlying bone.
The gums are composed of pale pink epithelial tissue that surrounds the cervical area of the teeth. Their texture is similar to the peel of an orange and they have sharp and precise edges.
When the gums change color, swell, bleed, or hurt, this indicates that something isn’t right. The main enemy of gingival tissue is the bacterial plaque that causes its irritation and inflammation.
In any case, there are other situations that also affect the health of the gingival mucosa. Let’s take a look at the 4 most frequent gum diseases in detail.
1. Gingivitis
Gingivitis is the most common and frequent disease of the gingival tissue. In fact, it’s also known as gum disease, as if it were the only disorder that affects gums.
The most common cause of gingivitis is the accumulation of bacterial plaque on the surfaces of the teeth and gums. This sticky film, invisible at first and whitish afterward, is made up mainly of bacteria and food debris.
When not properly removed through oral hygiene, plaque builds up. It can even calcify with the minerals in the mouth, giving rise to tartar or dental calculus.
Calculus and the toxins produced by plaque bacteria irritate and damage the gums. This triggers an inflammatory process, responsible for the symptoms of the disease. In addition to the above, there are other factors that can also cause inflammation of the gums:
- Genetic predisposition
- Hormonal changes such as puberty and pregnancy
- The use of orthodontics and prosthetics
- Smoking/tobacco
- Nutritional deficiencies
- Some medical conditions
- The consumption of certain medications
The symptoms of gingivitis and its treatment
It’s easy to identify the symptoms of gingivitis:
- Swelling of the gum tissue
- Dark red gums
- Tenderness or pain
- Bleeding at the slightest contact, especially during tooth brushing
- Bad breath
Being attentive to the appearance of the gums is what allows people to notice that something isn’t right in their mouth. When identifying any of the manifestations that we mention here, it’s important to seek a solution to the problem to prevent it from progressing.
To prevent and treat this disease, you need to control and eliminate bacterial plaque and tartar. On the one hand, it will be necessary to carry out professional cleaning every 6 or 12 months.
In addition, daily and frequent oral hygiene must be performed with the proper technique. This includes brushing with fluoride toothpastes, flossing, and using mouthwashes.
2. Periodontitis
Periodontitis or periodontal disease is the evolution of gingivitis that hasn’t been treated in time. The condition is deeper and compromises the tissues that support the teeth: The root cementum, periodontal ligament, and alveolar bone.
Between the edge of the gum and the dental tissue, pockets form that become larger and deeper over time. Inside, bacteria accumulate, causing an infectious focus that progresses until it completely destroys the supporting tissues.
Alveolar bone compromise is one of the most notorious complications of periodontitis. With bone loss, the teeth are no longer supported and begin to move. In the most advanced and serious cases, the teeth can be lost.
This condition, in addition to causing problems in the mouth, is associated with the appearance and complications of many systemic diseases. Diabetes, cardiovascular, neurological, and respiratory diseases are more aggressive in patients with periodontitis.
Periodontal disease during pregnancy is also a risk factor for complications during pregnancy. Premature deliveries, infants with low birth weight, and preeclampsia are associated with this oral condition.
Its treatment requires the intervention of a periodontist, who performs scraping and smoothing of the roots and a thorough professional cleaning. It’s also crucial to prescribe systemic antibiotics and antiseptics for local use, such as chlorhexidine. Some more serious cases may require periodontal surgeries to restore health to the affected tissues.
As in gingivitis, to prevent periodontitis, special emphasis must be placed on maintaining adequate oral hygiene and avoiding risk factors.
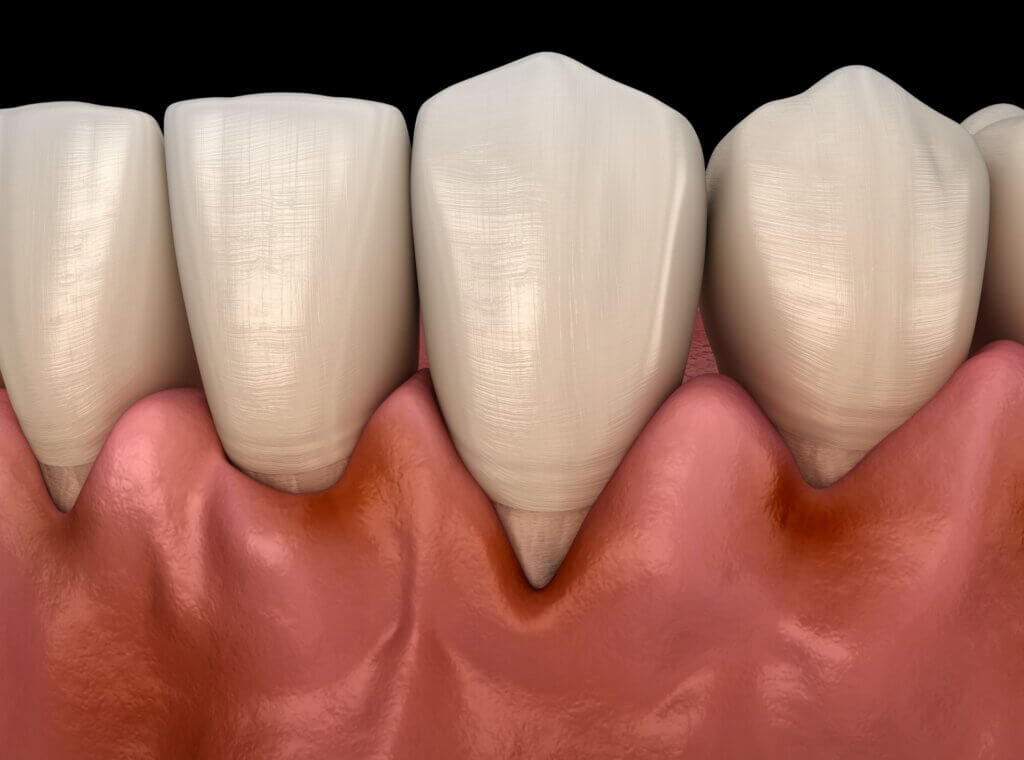
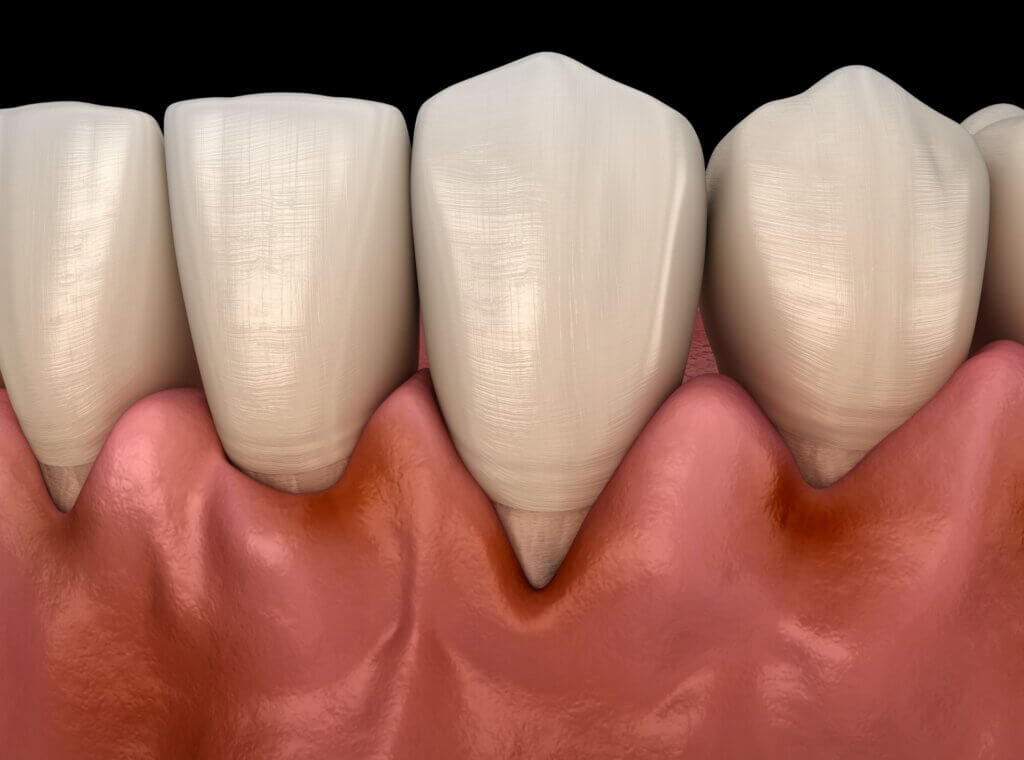
3. Gingival retraction
Another frequent gum disease is gingival recession. It’s the migration of this tissue to deeper areas, leaving part of the dental root uncovered.
The loss of gums generates dental sensitivity and increases the risk of cervical cavities. It also affects the aesthetics of the smile, giving the appearance of very long teeth.
Poor tooth brushing and the presence of periodontitis contribute to receding gums. However, it can also appear in people with adequate oral hygiene due to other causes:
- Hereditary factors: Some members of the same family have thinner gums and a greater predisposition to receding.
- Aging: The passing of time increases the chances that the gum tissue will recede.
- Smoking: The retraction of the gums is one of the many negative consequences of tobacco use in the mouth.
- Gingival tissue trauma from very vigorous tooth brushing, with a lot of pressure or with a hard bristle brush that injures the mucosa.
- Oral piercings: The presence of jewelry on the lips or on the tongue traumatizes the gums and causes them to recede.
- Misaligned or malpositioned teeth.
- Damages as a consequence of certain dental treatments.
Receding gums are visible to the naked eye, as the root of the tooth is exposed, which, as it doesn’t have its usual covering, looks longer. In addition, as a result of not having the gingival tissue as protection, the tooth can suffer sensitivity when eating something cold, sweet, or hot.
When gingival retraction is mild, the treatment consists of monitoring the situation so that it doesn’t progress. Effective but gentle tooth brushing and toothpastes for sensitive teeth help control symptoms.
The most complex cases may require different interventions to solve or improve the situation. Desensitizing agents, varnishes, dental restorations, covers, veneers, orthodontics, and surgeries are some of the alternatives.
4. Gingival hyperplasia
Gingival hyperplasia is the enlargement and exaggerated growth of the gums. This larger size of the gingival tissue may be associated with different factors:
- Genetics
- Gingival inflammation due to periodontitis
- Systemic conditions: Hormonal imbalances, leukemias
- The use of certain medications: Some anticonvulsants, immunosuppressants for transplant patients, and calcium channel blockers used to treat cardiovascular problems such as hypertension can cause gingival enlargement
In any case, poor oral hygiene and the accumulation of bacterial plaque worsen the situation.
There’s a type of gingival enlargement associated with pregnancy called a pyogenic granuloma. It’s a benign tumor that appears in the gums of pregnant women as a result of hormonal changes and increased body irrigation typical of pregnancy.
In general, this type of tumor subsides on its own after delivery. However, if the lesion bothers a woman a lot, a dentist can remove it with a simple surgery.
When gingival hyperplasia occurs, it’s important to determine the cause of the enlargement. Depending on the diagnosis, treatment varies.
In some cases, addressing hyperplasia with periodontal treatment and improvements in oral hygiene is necessary. If the cause is a medication, its substitution should be considered, consulting the health professional who prescribed it. Some cases require the removal of excess tissue through simple gum contouring surgery.
Recognize the most frequent gum diseases and find a solution
Now that you know the 4 most frequent gum diseases, you’ll be able to identify them if you notice their symptoms and seek help in a timely manner. Acting promptly avoids complications, not only at the oral level but in a person’s overall health.
Taking care of the gum tissue with proper oral hygiene and regular dental check-ups allows for a healthy mouth. Consequently, complications and more difficult and expensive treatments are avoided. This translates into gains in well-being, comfort, health, and aesthetics.
The most frequent gum diseases can put the permanence of the teeth in the mouth at risk. Other conditions compromise the aesthetics of the smile and cause discomfort and pain.
Gingival tissue has the function of protecting and supporting the teeth. Knowing the diseases that affect the gums will allow you to prevent them and take care of this area of the mouth.
Several pathological processes can develop in the gingival tissue. Today, we’ll tell you about the 4 most frequent gum diseases and how to avoid them.
What are the gums and how do the most common gum diseases occur?
The gums are the oral mucosa that surrounds each of the teeth in the mouth, covering the bone that supports them. They function as a protective barrier that prevents bacteria or foreign substances from entering the root area.
Gingival tissue helps teeth remain firm and fixed in the jaws. In addition, it acts as a buffer against the forces that are generated in the mouth, preventing its impact on the underlying bone.
The gums are composed of pale pink epithelial tissue that surrounds the cervical area of the teeth. Their texture is similar to the peel of an orange and they have sharp and precise edges.
When the gums change color, swell, bleed, or hurt, this indicates that something isn’t right. The main enemy of gingival tissue is the bacterial plaque that causes its irritation and inflammation.
In any case, there are other situations that also affect the health of the gingival mucosa. Let’s take a look at the 4 most frequent gum diseases in detail.
1. Gingivitis
Gingivitis is the most common and frequent disease of the gingival tissue. In fact, it’s also known as gum disease, as if it were the only disorder that affects gums.
The most common cause of gingivitis is the accumulation of bacterial plaque on the surfaces of the teeth and gums. This sticky film, invisible at first and whitish afterward, is made up mainly of bacteria and food debris.
When not properly removed through oral hygiene, plaque builds up. It can even calcify with the minerals in the mouth, giving rise to tartar or dental calculus.
Calculus and the toxins produced by plaque bacteria irritate and damage the gums. This triggers an inflammatory process, responsible for the symptoms of the disease. In addition to the above, there are other factors that can also cause inflammation of the gums:
- Genetic predisposition
- Hormonal changes such as puberty and pregnancy
- The use of orthodontics and prosthetics
- Smoking/tobacco
- Nutritional deficiencies
- Some medical conditions
- The consumption of certain medications
The symptoms of gingivitis and its treatment
It’s easy to identify the symptoms of gingivitis:
- Swelling of the gum tissue
- Dark red gums
- Tenderness or pain
- Bleeding at the slightest contact, especially during tooth brushing
- Bad breath
Being attentive to the appearance of the gums is what allows people to notice that something isn’t right in their mouth. When identifying any of the manifestations that we mention here, it’s important to seek a solution to the problem to prevent it from progressing.
To prevent and treat this disease, you need to control and eliminate bacterial plaque and tartar. On the one hand, it will be necessary to carry out professional cleaning every 6 or 12 months.
In addition, daily and frequent oral hygiene must be performed with the proper technique. This includes brushing with fluoride toothpastes, flossing, and using mouthwashes.
2. Periodontitis
Periodontitis or periodontal disease is the evolution of gingivitis that hasn’t been treated in time. The condition is deeper and compromises the tissues that support the teeth: The root cementum, periodontal ligament, and alveolar bone.
Between the edge of the gum and the dental tissue, pockets form that become larger and deeper over time. Inside, bacteria accumulate, causing an infectious focus that progresses until it completely destroys the supporting tissues.
Alveolar bone compromise is one of the most notorious complications of periodontitis. With bone loss, the teeth are no longer supported and begin to move. In the most advanced and serious cases, the teeth can be lost.
This condition, in addition to causing problems in the mouth, is associated with the appearance and complications of many systemic diseases. Diabetes, cardiovascular, neurological, and respiratory diseases are more aggressive in patients with periodontitis.
Periodontal disease during pregnancy is also a risk factor for complications during pregnancy. Premature deliveries, infants with low birth weight, and preeclampsia are associated with this oral condition.
Its treatment requires the intervention of a periodontist, who performs scraping and smoothing of the roots and a thorough professional cleaning. It’s also crucial to prescribe systemic antibiotics and antiseptics for local use, such as chlorhexidine. Some more serious cases may require periodontal surgeries to restore health to the affected tissues.
As in gingivitis, to prevent periodontitis, special emphasis must be placed on maintaining adequate oral hygiene and avoiding risk factors.
3. Gingival retraction
Another frequent gum disease is gingival recession. It’s the migration of this tissue to deeper areas, leaving part of the dental root uncovered.
The loss of gums generates dental sensitivity and increases the risk of cervical cavities. It also affects the aesthetics of the smile, giving the appearance of very long teeth.
Poor tooth brushing and the presence of periodontitis contribute to receding gums. However, it can also appear in people with adequate oral hygiene due to other causes:
- Hereditary factors: Some members of the same family have thinner gums and a greater predisposition to receding.
- Aging: The passing of time increases the chances that the gum tissue will recede.
- Smoking: The retraction of the gums is one of the many negative consequences of tobacco use in the mouth.
- Gingival tissue trauma from very vigorous tooth brushing, with a lot of pressure or with a hard bristle brush that injures the mucosa.
- Oral piercings: The presence of jewelry on the lips or on the tongue traumatizes the gums and causes them to recede.
- Misaligned or malpositioned teeth.
- Damages as a consequence of certain dental treatments.
Receding gums are visible to the naked eye, as the root of the tooth is exposed, which, as it doesn’t have its usual covering, looks longer. In addition, as a result of not having the gingival tissue as protection, the tooth can suffer sensitivity when eating something cold, sweet, or hot.
When gingival retraction is mild, the treatment consists of monitoring the situation so that it doesn’t progress. Effective but gentle tooth brushing and toothpastes for sensitive teeth help control symptoms.
The most complex cases may require different interventions to solve or improve the situation. Desensitizing agents, varnishes, dental restorations, covers, veneers, orthodontics, and surgeries are some of the alternatives.
4. Gingival hyperplasia
Gingival hyperplasia is the enlargement and exaggerated growth of the gums. This larger size of the gingival tissue may be associated with different factors:
- Genetics
- Gingival inflammation due to periodontitis
- Systemic conditions: Hormonal imbalances, leukemias
- The use of certain medications: Some anticonvulsants, immunosuppressants for transplant patients, and calcium channel blockers used to treat cardiovascular problems such as hypertension can cause gingival enlargement
In any case, poor oral hygiene and the accumulation of bacterial plaque worsen the situation.
There’s a type of gingival enlargement associated with pregnancy called a pyogenic granuloma. It’s a benign tumor that appears in the gums of pregnant women as a result of hormonal changes and increased body irrigation typical of pregnancy.
In general, this type of tumor subsides on its own after delivery. However, if the lesion bothers a woman a lot, a dentist can remove it with a simple surgery.
When gingival hyperplasia occurs, it’s important to determine the cause of the enlargement. Depending on the diagnosis, treatment varies.
In some cases, addressing hyperplasia with periodontal treatment and improvements in oral hygiene is necessary. If the cause is a medication, its substitution should be considered, consulting the health professional who prescribed it. Some cases require the removal of excess tissue through simple gum contouring surgery.
Recognize the most frequent gum diseases and find a solution
Now that you know the 4 most frequent gum diseases, you’ll be able to identify them if you notice their symptoms and seek help in a timely manner. Acting promptly avoids complications, not only at the oral level but in a person’s overall health.
Taking care of the gum tissue with proper oral hygiene and regular dental check-ups allows for a healthy mouth. Consequently, complications and more difficult and expensive treatments are avoided. This translates into gains in well-being, comfort, health, and aesthetics.
- Taboada-Aranza, O., Cerón Argüelles, J., & Rodríguez Hernández, A. (2018). Frecuencia y distribución de enfermedades periodontales asociadas a placa bacteriana en pacientes que acuden a una clínica universitaria. Rev ADM, 75(3), 147-52.
- Rathee, M., & Jain, P. (2022). Gingivitis. In StatPearls [Internet]. StatPearls Publishing.
- Matesanz-Pérez, P., Matos-Cruz, R., & Bascones-Martínez, A. (2008). Enfermedades gingivales: una revisión de la literatura. Avances en periodoncia e implantologia oral, 20(1), 11-25.
- Khumaedi, A. I., Purnamasari, D., Wijaya, I. P., & Soeroso, Y. (2019). The relationship of diabetes, periodontitis and cardiovascular disease. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 13(2), 1675-1678.
- Jajoo, N. S., Shelke, A. U., Bajaj, R. S., Patil, P. P., & Patil, M. A. (2020). Association of periodontitis with pre term low birth weight–A review. Placenta, 95, 62-68.
- Pockpa, Z. A. D., Soueidan, A., Koffi-Coulibaly, N. T., Limam, A., Badran, Z., & Struillou, X. (2021). Periodontal diseases and adverse pregnancy outcomes: review of two decades of clinical research. Oral Health Prev Dent, 19(1), 77-83.
- Chaguay Alvarado, J. S. (2021). El tabaquismo y sus consecuencias en la cavidad bucal (Bachelor’s thesis, Universidad de Guayaquil. Facultad Piloto de Odontología).
- Nieto Sánchez, V. (2020). Recesiones gingivales en ortodoncia. Revisión sistemática.
- Cacciola, D., & Gómez, G. M. (2018). Relación entre periodoncia y ortodoncia: complicaciones gingivales y efectos del tratamiento ortodóncico en el periodonto. Biociencias, 13(2).
- Guerra, J., Montenegro, M. G., & Ureña, E. (2021). Hiperplasia Gingival Inducida por Fármacos. Contacto Científico, 1(1), 27-37.
- Mendoza Vásquez, S. S. (2022). Granuloma piógeno en mujeres embarazadas.
- Gomez Melgarejo, D. M. (2022). Gingivectomia con gingivoplastia en incisivos superiores.
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.







