Differences Between Bronchitis and Pneumonia


Escrito y verificado por el biólogo Samuel Antonio Sánchez Amador
Respiratory diseases are a very serious global health problem. As indicated by the World Health Organization (WHO), several of them are among the 10 pathologies that cause the most annual deaths. Knowing the differences between conditions such as bronchitis and pneumonia is essential in order to prevent the progression of the diseases and even the death of the patients.
Although they’re sometimes used as interchangeable terms, in reality these two medical concepts are quite different from each other. The difference lies, above all, in the area of the respiratory tree where the infectious focus occurs. If you want to know more about this group of prevalent pathologies, keep reading.
What are respiratory diseases?
Before explaining the differences between the two conditions, we need to establish that both bronchitis and pneumonia are included in the group of respiratory diseases. All of them, together, are pathological conditions that affect the organs responsible for carrying out respiratory exchange with the environment.
These diseases can affect the trachea, bronchi, bronchioles, alveoli, pleura, pleural cavity, and nerve (or muscle) endings responsible for the mechanical act of breathing. The WHO and other sources show us the importance of these pathologies with the following data:
- In recent decades there has been a marked increase in deaths and disability due to chronic respiratory diseases.
- These conditions are a serious public health problem, since, in 2017 alone, they caused 3.9 million deaths, 7% of all deaths. In the United States, this figure rises to 7.5%.
- Chronic obstructive pulmonary disease (COPD) and respiratory tract infections are the third and fourth leading causes of death worldwide, second only to ischemic heart disease and strokes.
- About 65 million people in the world have COPD. 334 million inhabitants suffer from asthma, which makes this pathology the most common chronic condition in childhood (14% of the child population experiences it).
Respiratory diseases cause not inconsiderable morbidity and mortality, especially in low-income countries and in vulnerable groups. Therefore, it’s essential to know how to distinguish between the different conditions before the patient’s prognosis worsens.
What are the differences between bronchitis and pneumonia?
Bronchitis and pneumonia are respiratory diseases with quite a few differences. Next, we’ll explore their differences by section, ranging from etiology to treatment.
1. Different places of origin
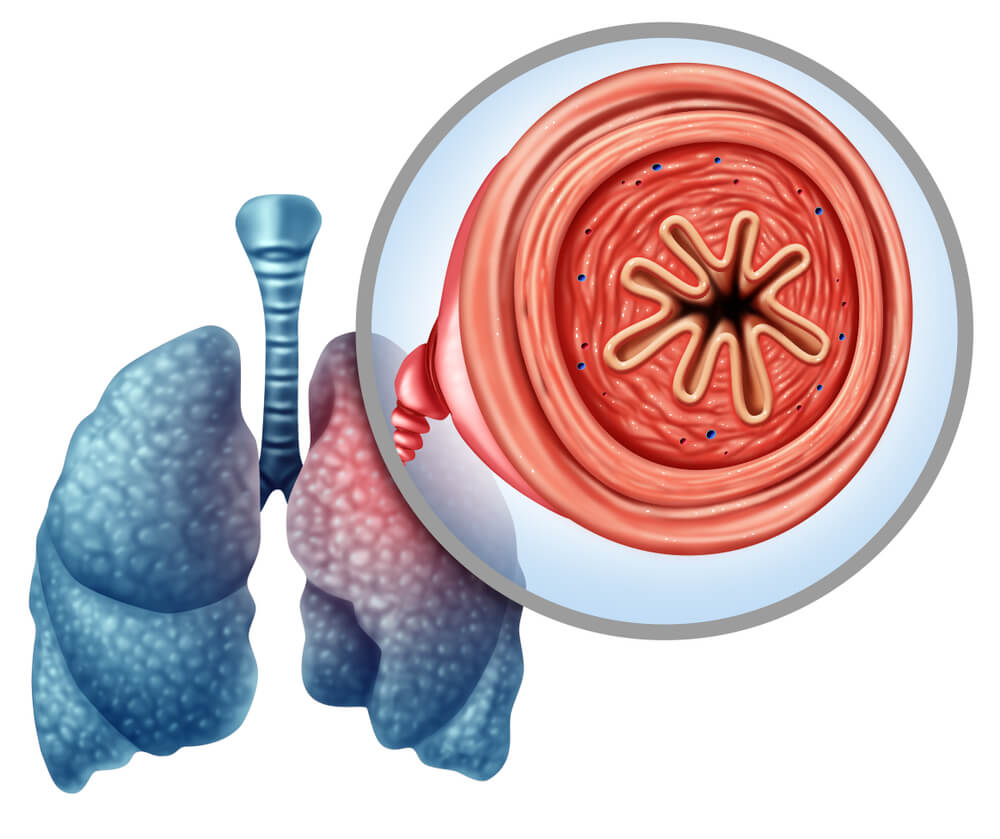
One of the main differences between bronchitis and pneumonia lies in the area of infection. As indicated by the Healthline medical portal, bronchitis causes inflammation in the bronchi, while pneumonia primarily affects the alveoli.
The main bronchi are 2 tubes that branch off from the trachea at the level of the fourth or fifth thoracic vertebra, and are responsible for transporting air to and from the lungs. After division, each of these ducts enters the lung parenchyma and is subdivided into much smaller branches of a millimeter or less, the bronchioles.
Finally, the bronchioles flow into the alveoli. The National Cancer Institute defines these structures as ‘tiny air-filled pockets in which gas exchange (of O₂ and CO₂) occurs between the lung and blood during air respiration.’ Each alveolus measures 200 microns in diameter and is delimited by a wall made up of thin cells (pneumocytes).
The terms bronchi, bronchioles, and alveoli are complementary, since they’re all part of the human respiratory chain. We can summarize the difference between bronchitis and pneumonia in this area with the following concepts:
- Bronchitis: An inflammation that occurs in the inner lining of the bronchial tubes. It’s characterized by marked respiratory distress and excretion of mucus.
- Pneumonia: In pneumonia, inflammation occurs in the air sacs (alveoli) of one or both lungs. This condition can vary greatly in severity and ranges from mild to life-threatening.
2. Bronchitis comes in two different types
Another difference between bronchitis and pneumonia lies in the division of the condition according to its duration. Pneumonia isn’t usually conceived as chronic in all cases, as it’s almost always caused by infectious agents and the course of the disease is rapid. An exception to this rule is chronic eosinophilic pneumonia (NEC), but we won’t discuss this here.
On the other hand, bronchitis is diagnosed as acute or chronic depending on its duration. We’re going to show you in the following sections the clinical characteristics of each variant.
Acute bronchitis
As its name suggests, acute bronchitis is inflammation of the bronchial tubes for a short period (3 weeks or less). It’s the most common type of bronchitis and in 90% of cases its cause lies in viral infections. Studies from the United States estimate that 5% of the US population has an episode of this type per year, which translates into 10 million annual medical visits.
Although viruses are the most common causative agents, this condition can also be caused by allergens, pollution, and irritating chemicals. Acute inflammation of the bronchial walls results in the thickening of the mucosa, desquamation of epithelial cells, and denudation of the basement membrane.
Acute bronchitis lasts about 3 weeks.
Chronic bronchitis
The premise of chronic bronchitis is the same as acute, but it lasts much longer. By definition, symptoms must be present for at least 3 months for 2 consecutive years to diagnose it. The etiology is very different from the previous case, as in this condition the inflammation of the bronchi can’t be attributed to a viral picture.
As indicated in the portal Statpearls, this type of bronchitis is due to overstimulation and overproduction of mucus by goblet cells of the bronchi. In addition, these pictures show how epithelial cells respond to exposure to toxins (such as tobacco smoke) by secreting inflammatory agents, such as interleukin 8.
When chronic bronchitis is accompanied by reduced airflow, the condition is called Chronic Obstructive Pulmonary Disease (COPD). Many people with chronic bronchitis go on to develop COPD, but not all people with COPD also have the chronic bronchial inflammation typical of bronchitis.
In summary, chronic bronchitis is slower onset but of much longer duration.
3. The duration of illnesses varies
Now that we have described acute bronchitis and chronic bronchitis, we find it interesting to compare these pathological variants with respect to pneumonia in terms of temporal extension. In the following list we summarize the figures of greatest interest:
- Chronic bronchitis: As we have said, this condition occurs frequently every 3 months for at least 2 years. Symptoms can be improved, but are never fully cured.
- Acute bronchitis: Acute bronchitis has an average duration of 2 to 3 weeks. Although the cough may remain for a month or more, it shouldn’t get worse in the later stages of the disease.
- Pneumonia: Depending on the causative agent and the patient, pneumonia can last for one to several weeks. In any case, its general duration is less than that of bronchitis, especially if we compare it with the chronic variety.
4. Different causes
The causative agents are different in bronchitis and pneumonia. As we have said, 90% of acute bronchial symptoms are due to viral agents, while 50% of community-acquired pneumonia are caused by the bacterial agent Streptococcus pneumoniae. One variant is eminently viral and the other bacterial.
Acute bronchitis is usually caused by respiratory syncytial virus, influenza trigger viruses (influenza A and influenza B), rhinoviruses, and other biological agents common in the general population. Bacterial triggers are very rare, but the Mycoplasma pneumoniae, Chlamydophila pneumonia, and Bordetella pertussis species, among others, should be highlighted.
Chronic bronchitis isn’t triggered by a viral or bacterial agent, as the most common respiratory tract infections don’t last as long. Tobacco use is one of the most common causes, since up to 75% of people who end up developing this condition were smoking at the time of diagnosis. Exposure to other chemicals also promotes it.
In contrast, half of the pneumonia cases contracted outside hospitals are due to S. pneumoniae. The remaining 20% of cases are caused by Haemophilus influenzae and 13% respond to a Chlamydophila pneumoniae infection. There are antibiotic-resistant strains of some of these pathogens, making treatment very difficult.
Finally, it should be noted that up to 1/3 of pneumonia cases can be caused by viral agents (and there are some non-infectious variants). Rhinoviruses, coronaviruses, influenza viruses, and respiratory syncytial virus are some of the most common. Interestingly, these same agents have been cited to describe the etiology of acute bronchitis.
Acute bronchitis is almost always caused by viruses and pneumonia by bacteria. However, both share pathogens with each other. Chronic bronchitis, meanwhile, is explained by exposure to harmful chemical agents.
5. Differential symptoms
Although both are respiratory diseases, bronchitis and pneumonia appear with quite different symptoms (and of variable duration). In the following list, we compare each pathology of interest according to its signology:
- Acute bronchitis: A productive cough, malaise, shortness of breath, and wheezing. Cough is the main complaint of patients and is accompanied by the excretion of mucous sputum, usually of a light or yellowish color. The cough lasts on average 10-20 days after the resolution of the condition, although it can last for up to 4 weeks. Catarrhal symptoms are also common.
- Chronic bronchitis: Coughing (productive in 50% of cases, but not always), wheezing, “rasping” sounds when breathing, shortness of breath, and a chronic feeling of tightness in the chest. If there’s sputum, it may be yellowish, green, and even stained with blood.
- Chronic bronchitis complicated with COPD: All of the above symptoms, plus weight loss, lack of energy, and swelling of the ankles, feet, and legs.
- Pneumonia: Chest pain when breathing or coughing, disorientation, phlegmy cough, fatigue, fever, chills, tremor, nausea, vomiting, and shortness of breath.
All of this terminology may sound complicated, but the distinctions are straightforward. Acute bronchitis usually presents with mild-moderate forms and is often accompanied by catarrhal symptoms (since it’s almost always caused by viruses). As the condition worsens (in its chronic variant or COPD) the sputum may turn bloody and the shortness of breath is more evident.
Instead, pneumonia usually has symptoms that are more typical of a bacterial infection. The fever is higher, the chest pain is more evident, and vomiting, nausea, and chills are more common. In addition, clinical signs of catarrh (such as a stuffy nose or throat clearing) aren’t expected here.
6. Different treatments

It isn’t easy to talk about the differences between bronchitis and pneumonia when it comes to treatment, as each condition can have many causes. As you can imagine, the medical approach to acute viral bronchitis differs greatly from that used to alleviate COPD or resolve bacterial pneumonia. Because of this, we’ll keep things simple (and general).
As the Mayo Clinic indicates, most cases of acute bronchitis don’t require specific treatment, as they’re caused by viruses. You just have to wait for the patient’s immune system to fight the infection and the symptoms disappear. If the cough is very bothersome, cough suppressants can be used, but little else. Hospitalization isn’t usually necessary.
On the other hand, pneumonia does require the use of antibiotics in many cases (as long as it’s caused by bacteria). Amoxicillin, doxycycline, and macrolides are the drugs that are prescribed almost systematically, as it’s necessary to start treating it as soon as possible. Unfortunately, this sometimes leads to the overuse of antibiotics as the right type is often not chosen straight away.
If the condition doesn’t improve, the patient’s treatment must be changed and newer antibiotics (or a combination of two of them) must be sought. In some cases, hospitalization and oxygen therapy are necessary (especially in older people).
Chronic bronchitis is mostly treated with bronchodilators and lifestyle changes. As we have said in previous lines, full recovery is often not possible in this case.
A very complex pathological group
Talking about the differences between bronchitis and pneumonia is complex. Both conditions are very general and can be caused by viruses, bacteria, other microorganisms, and even non-infectious agents (such as chemicals). However, the main distinction is clear: acute bronchitis is almost always viral, and pneumonia is bacterial.
Acute bronchitis usually heals on its own, while pneumonia requires the application of generic or specific antibiotics. On the other hand, conditions such as chronic bronchitis and COPD have no solution, although it is possible to improve the patient’s quality of life with supportive therapies.
Respiratory diseases are a very serious global health problem. As indicated by the World Health Organization (WHO), several of them are among the 10 pathologies that cause the most annual deaths. Knowing the differences between conditions such as bronchitis and pneumonia is essential in order to prevent the progression of the diseases and even the death of the patients.
Although they’re sometimes used as interchangeable terms, in reality these two medical concepts are quite different from each other. The difference lies, above all, in the area of the respiratory tree where the infectious focus occurs. If you want to know more about this group of prevalent pathologies, keep reading.
What are respiratory diseases?
Before explaining the differences between the two conditions, we need to establish that both bronchitis and pneumonia are included in the group of respiratory diseases. All of them, together, are pathological conditions that affect the organs responsible for carrying out respiratory exchange with the environment.
These diseases can affect the trachea, bronchi, bronchioles, alveoli, pleura, pleural cavity, and nerve (or muscle) endings responsible for the mechanical act of breathing. The WHO and other sources show us the importance of these pathologies with the following data:
- In recent decades there has been a marked increase in deaths and disability due to chronic respiratory diseases.
- These conditions are a serious public health problem, since, in 2017 alone, they caused 3.9 million deaths, 7% of all deaths. In the United States, this figure rises to 7.5%.
- Chronic obstructive pulmonary disease (COPD) and respiratory tract infections are the third and fourth leading causes of death worldwide, second only to ischemic heart disease and strokes.
- About 65 million people in the world have COPD. 334 million inhabitants suffer from asthma, which makes this pathology the most common chronic condition in childhood (14% of the child population experiences it).
Respiratory diseases cause not inconsiderable morbidity and mortality, especially in low-income countries and in vulnerable groups. Therefore, it’s essential to know how to distinguish between the different conditions before the patient’s prognosis worsens.
What are the differences between bronchitis and pneumonia?
Bronchitis and pneumonia are respiratory diseases with quite a few differences. Next, we’ll explore their differences by section, ranging from etiology to treatment.
1. Different places of origin
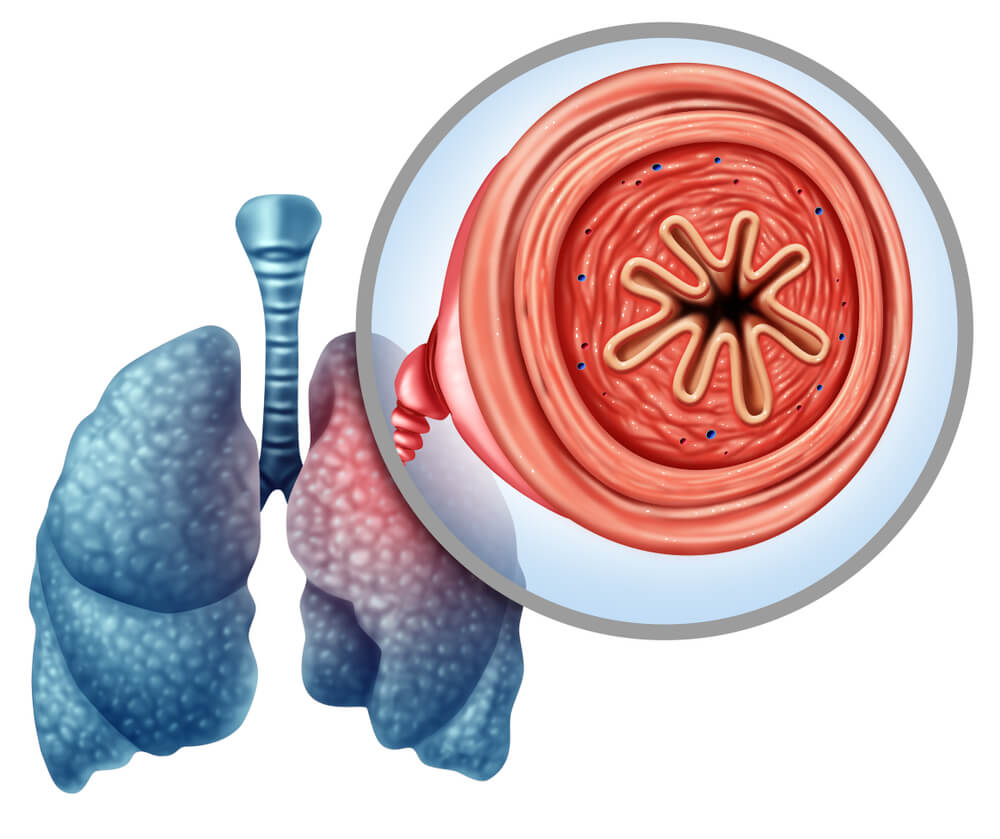
One of the main differences between bronchitis and pneumonia lies in the area of infection. As indicated by the Healthline medical portal, bronchitis causes inflammation in the bronchi, while pneumonia primarily affects the alveoli.
The main bronchi are 2 tubes that branch off from the trachea at the level of the fourth or fifth thoracic vertebra, and are responsible for transporting air to and from the lungs. After division, each of these ducts enters the lung parenchyma and is subdivided into much smaller branches of a millimeter or less, the bronchioles.
Finally, the bronchioles flow into the alveoli. The National Cancer Institute defines these structures as ‘tiny air-filled pockets in which gas exchange (of O₂ and CO₂) occurs between the lung and blood during air respiration.’ Each alveolus measures 200 microns in diameter and is delimited by a wall made up of thin cells (pneumocytes).
The terms bronchi, bronchioles, and alveoli are complementary, since they’re all part of the human respiratory chain. We can summarize the difference between bronchitis and pneumonia in this area with the following concepts:
- Bronchitis: An inflammation that occurs in the inner lining of the bronchial tubes. It’s characterized by marked respiratory distress and excretion of mucus.
- Pneumonia: In pneumonia, inflammation occurs in the air sacs (alveoli) of one or both lungs. This condition can vary greatly in severity and ranges from mild to life-threatening.
2. Bronchitis comes in two different types
Another difference between bronchitis and pneumonia lies in the division of the condition according to its duration. Pneumonia isn’t usually conceived as chronic in all cases, as it’s almost always caused by infectious agents and the course of the disease is rapid. An exception to this rule is chronic eosinophilic pneumonia (NEC), but we won’t discuss this here.
On the other hand, bronchitis is diagnosed as acute or chronic depending on its duration. We’re going to show you in the following sections the clinical characteristics of each variant.
Acute bronchitis
As its name suggests, acute bronchitis is inflammation of the bronchial tubes for a short period (3 weeks or less). It’s the most common type of bronchitis and in 90% of cases its cause lies in viral infections. Studies from the United States estimate that 5% of the US population has an episode of this type per year, which translates into 10 million annual medical visits.
Although viruses are the most common causative agents, this condition can also be caused by allergens, pollution, and irritating chemicals. Acute inflammation of the bronchial walls results in the thickening of the mucosa, desquamation of epithelial cells, and denudation of the basement membrane.
Acute bronchitis lasts about 3 weeks.
Chronic bronchitis
The premise of chronic bronchitis is the same as acute, but it lasts much longer. By definition, symptoms must be present for at least 3 months for 2 consecutive years to diagnose it. The etiology is very different from the previous case, as in this condition the inflammation of the bronchi can’t be attributed to a viral picture.
As indicated in the portal Statpearls, this type of bronchitis is due to overstimulation and overproduction of mucus by goblet cells of the bronchi. In addition, these pictures show how epithelial cells respond to exposure to toxins (such as tobacco smoke) by secreting inflammatory agents, such as interleukin 8.
When chronic bronchitis is accompanied by reduced airflow, the condition is called Chronic Obstructive Pulmonary Disease (COPD). Many people with chronic bronchitis go on to develop COPD, but not all people with COPD also have the chronic bronchial inflammation typical of bronchitis.
In summary, chronic bronchitis is slower onset but of much longer duration.
3. The duration of illnesses varies
Now that we have described acute bronchitis and chronic bronchitis, we find it interesting to compare these pathological variants with respect to pneumonia in terms of temporal extension. In the following list we summarize the figures of greatest interest:
- Chronic bronchitis: As we have said, this condition occurs frequently every 3 months for at least 2 years. Symptoms can be improved, but are never fully cured.
- Acute bronchitis: Acute bronchitis has an average duration of 2 to 3 weeks. Although the cough may remain for a month or more, it shouldn’t get worse in the later stages of the disease.
- Pneumonia: Depending on the causative agent and the patient, pneumonia can last for one to several weeks. In any case, its general duration is less than that of bronchitis, especially if we compare it with the chronic variety.
4. Different causes
The causative agents are different in bronchitis and pneumonia. As we have said, 90% of acute bronchial symptoms are due to viral agents, while 50% of community-acquired pneumonia are caused by the bacterial agent Streptococcus pneumoniae. One variant is eminently viral and the other bacterial.
Acute bronchitis is usually caused by respiratory syncytial virus, influenza trigger viruses (influenza A and influenza B), rhinoviruses, and other biological agents common in the general population. Bacterial triggers are very rare, but the Mycoplasma pneumoniae, Chlamydophila pneumonia, and Bordetella pertussis species, among others, should be highlighted.
Chronic bronchitis isn’t triggered by a viral or bacterial agent, as the most common respiratory tract infections don’t last as long. Tobacco use is one of the most common causes, since up to 75% of people who end up developing this condition were smoking at the time of diagnosis. Exposure to other chemicals also promotes it.
In contrast, half of the pneumonia cases contracted outside hospitals are due to S. pneumoniae. The remaining 20% of cases are caused by Haemophilus influenzae and 13% respond to a Chlamydophila pneumoniae infection. There are antibiotic-resistant strains of some of these pathogens, making treatment very difficult.
Finally, it should be noted that up to 1/3 of pneumonia cases can be caused by viral agents (and there are some non-infectious variants). Rhinoviruses, coronaviruses, influenza viruses, and respiratory syncytial virus are some of the most common. Interestingly, these same agents have been cited to describe the etiology of acute bronchitis.
Acute bronchitis is almost always caused by viruses and pneumonia by bacteria. However, both share pathogens with each other. Chronic bronchitis, meanwhile, is explained by exposure to harmful chemical agents.
5. Differential symptoms
Although both are respiratory diseases, bronchitis and pneumonia appear with quite different symptoms (and of variable duration). In the following list, we compare each pathology of interest according to its signology:
- Acute bronchitis: A productive cough, malaise, shortness of breath, and wheezing. Cough is the main complaint of patients and is accompanied by the excretion of mucous sputum, usually of a light or yellowish color. The cough lasts on average 10-20 days after the resolution of the condition, although it can last for up to 4 weeks. Catarrhal symptoms are also common.
- Chronic bronchitis: Coughing (productive in 50% of cases, but not always), wheezing, “rasping” sounds when breathing, shortness of breath, and a chronic feeling of tightness in the chest. If there’s sputum, it may be yellowish, green, and even stained with blood.
- Chronic bronchitis complicated with COPD: All of the above symptoms, plus weight loss, lack of energy, and swelling of the ankles, feet, and legs.
- Pneumonia: Chest pain when breathing or coughing, disorientation, phlegmy cough, fatigue, fever, chills, tremor, nausea, vomiting, and shortness of breath.
All of this terminology may sound complicated, but the distinctions are straightforward. Acute bronchitis usually presents with mild-moderate forms and is often accompanied by catarrhal symptoms (since it’s almost always caused by viruses). As the condition worsens (in its chronic variant or COPD) the sputum may turn bloody and the shortness of breath is more evident.
Instead, pneumonia usually has symptoms that are more typical of a bacterial infection. The fever is higher, the chest pain is more evident, and vomiting, nausea, and chills are more common. In addition, clinical signs of catarrh (such as a stuffy nose or throat clearing) aren’t expected here.
6. Different treatments

It isn’t easy to talk about the differences between bronchitis and pneumonia when it comes to treatment, as each condition can have many causes. As you can imagine, the medical approach to acute viral bronchitis differs greatly from that used to alleviate COPD or resolve bacterial pneumonia. Because of this, we’ll keep things simple (and general).
As the Mayo Clinic indicates, most cases of acute bronchitis don’t require specific treatment, as they’re caused by viruses. You just have to wait for the patient’s immune system to fight the infection and the symptoms disappear. If the cough is very bothersome, cough suppressants can be used, but little else. Hospitalization isn’t usually necessary.
On the other hand, pneumonia does require the use of antibiotics in many cases (as long as it’s caused by bacteria). Amoxicillin, doxycycline, and macrolides are the drugs that are prescribed almost systematically, as it’s necessary to start treating it as soon as possible. Unfortunately, this sometimes leads to the overuse of antibiotics as the right type is often not chosen straight away.
If the condition doesn’t improve, the patient’s treatment must be changed and newer antibiotics (or a combination of two of them) must be sought. In some cases, hospitalization and oxygen therapy are necessary (especially in older people).
Chronic bronchitis is mostly treated with bronchodilators and lifestyle changes. As we have said in previous lines, full recovery is often not possible in this case.
A very complex pathological group
Talking about the differences between bronchitis and pneumonia is complex. Both conditions are very general and can be caused by viruses, bacteria, other microorganisms, and even non-infectious agents (such as chemicals). However, the main distinction is clear: acute bronchitis is almost always viral, and pneumonia is bacterial.
Acute bronchitis usually heals on its own, while pneumonia requires the application of generic or specific antibiotics. On the other hand, conditions such as chronic bronchitis and COPD have no solution, although it is possible to improve the patient’s quality of life with supportive therapies.
- The top 10 causes of death, Organización Mundial de la Salud (OMS). Recogido a 17 de septiembre en https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
- El impacto mundial de la enfermedad respiratoria, OMS. Recogido a 17 de septiembre en https://www.healthline.com/health/bronchitis-vs-pneumonia
- Alveolo, NIH. Recogido a 17 de septiembre en https://www.cancer.gov/espanol/publicaciones/diccionarios/diccionario-cancer/def/alveolos
- Singh, A., Avula, A., & Zahn, E. (2021). Acute bronchitis. StatPearls [Internet].
- Widysanto, A., & Mathew, G. (2020). Chronic Bronchitis. StatPearls [Internet].
- Bronquitis, Mayoclinic. Recogido a 17 de septiembre en https://www.mayoclinic.org/es-es/diseases-conditions/bronchitis/diagnosis-treatment/drc-20355572
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.







