Escitalopram: A Serotonin Reuptake Inhibitor
Escitalopram is a drug that has antidepressant properties. Therefore, it’s indicated in the treatment of depression and is a serotonin reuptake inhibitor, meaning it’s related to other drugs in this group with which it shares many characteristics. Some examples of these are fluoxetine and paroxetine.
Escitalopram was developed jointly by Lundbeck and Forest laboratories. Its development began in the summer of 1997, achieving its preparation and application for approval by the US FDA in March 2001.
The short development period can be attributed to the extensive experience of Lundbeck and Forest in the development of another drug with similar pharmacological properties, citalopram.
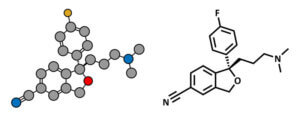
At the same time, escitalopram is the S enantiomer of citalopram, hence its rapid development. Enantiomers are a class of molecules in which in the pair of compounds, the molecule of one is a mirror image of the molecule of the other and they’re not superimposable.
Throughout the article, we’ll talk about the following aspects related to escitalopram:
- What is depression? What about serotonin?
- The mechanism of action.
- Pharmacokinetics.
- Indications and dosage.
- Adverse reactions and contraindications.
What is depression? What about serotonin?
As we’ve mentioned, escitalopram is used mainly for the treatment of depression by inhibiting the reuptake of serotonin. However, if we don’t understand these two terms well, we won’t be able to understand how this drug works.
Therefore, depression is a severe clinical illness with constant states of sadness. However, it goes further. It’s a disorder of the brain and there are many causes of its development, including genetic, biological, environmental, and psychological factors.

Among the biological factors, we can highlight that depression is associated with a deficit of the neurotransmitter serotonin. This chemical is made by the body and transmits signals between nerves, which is why it’s a neurotransmitter.
Serotonin is considered by some researchers to be the chemical responsible for maintaining the balance of our mood. Therefore, a deficit of serotonin leads to depressive states.
The mechanism of action of escitalopram
As we already know, it’s a serotonin reuptake inhibitor. Furthermore, it’s highly selective with minimal effects on the reuptake of norepinephrine and dopamine, two other neurotransmitters.
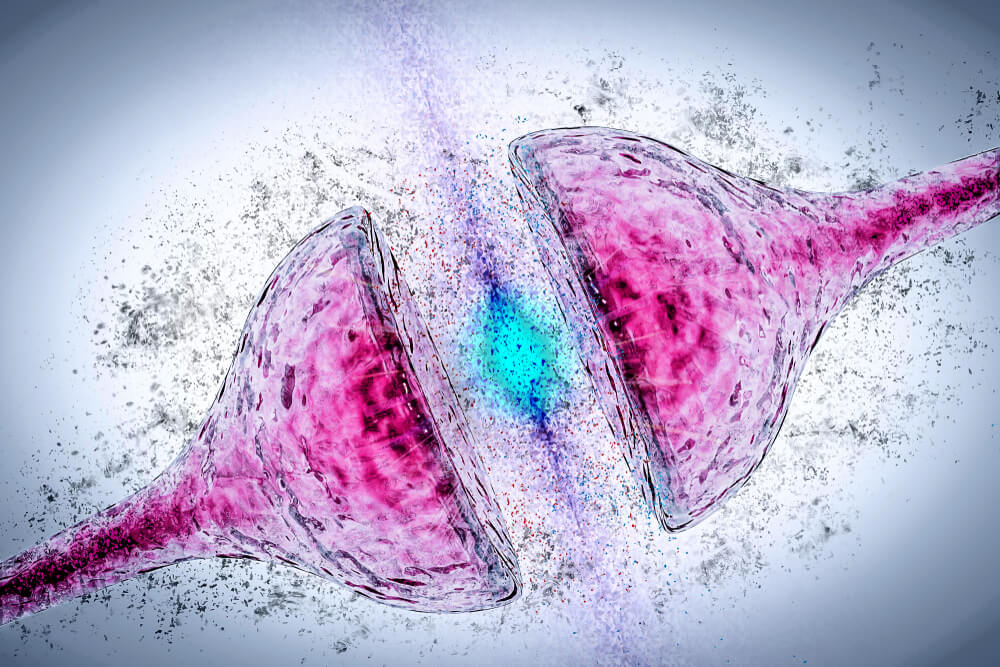
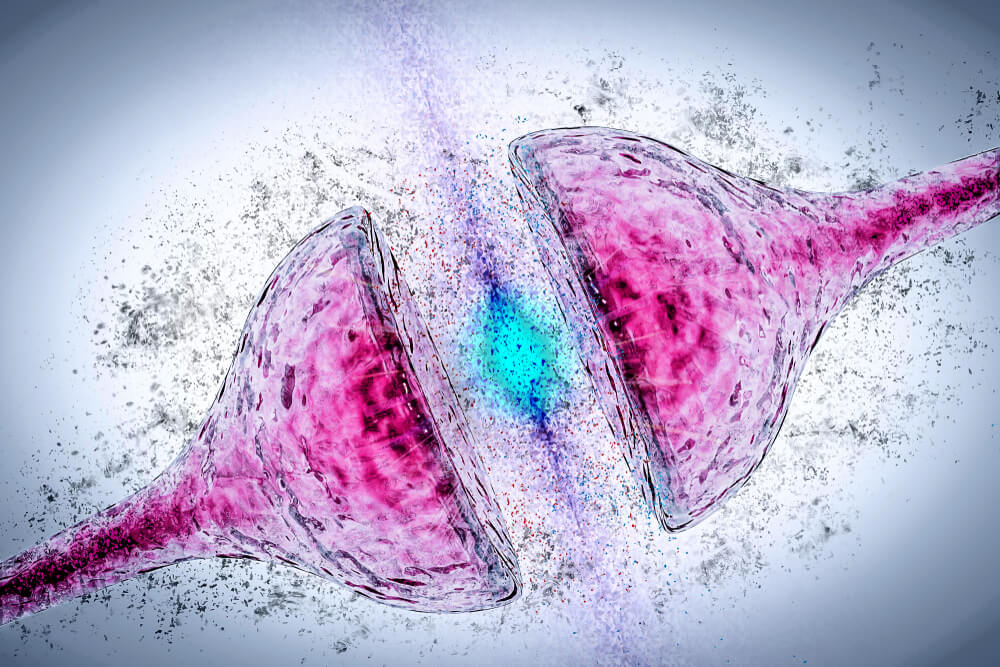
In other words, serotonin, like other neurotransmitters, is secreted by one neuron to bind with receptors on the membrane of another neighboring neuron and trigger an effect.
Later, it’s released from this receptor and some molecules return to the neuron that previously secreted it through a reuptake process.
It’s in this process where escitalopram acts, which inhibits it. By inhibiting it, the reuptake process of serotonin doesn’t take place and its concentration increases in the space between one neuron and another known as the presynaptic space. As there’s more serotonin, it can reattach to receptors on the neuron’s membrane and trigger more effect.
Escitalopram is at least 100 times more potent than the R enantiomer as a serotonin reuptake inhibitor and as an inhibitor of neuronal serotonin transport.
In addition, it has a low, almost zero, affinity for other types of biological amine receptors, which would explain why it has fewer adverse effects than other serotonin reuptake inhibitor drugs. This process is the only probable mechanism of action that explains the pharmacological and clinical effects of escitalopram.
Escitalopram pharmacokinetics
Within pharmacokinetics, which are the different processes and changes that the drug undergoes in the body, to put it in a simplified way, we’ll see the following aspects: Absorption, distribution, metabolism, and elimination.
Absorption
When the drug is administered orally, absorption is almost complete. Also, it doesn’t vary with food intake. Bioavailability, which is the actual concentration of the drug that will trigger the effect, is around 80%.
You may be interested: The Role of Serotonin in Depression
Distribution
This drug is distributed throughout the body, bound to plasma proteins in a percentage lower than 80%. This information is important to take into account if you’re taking another drug with a high degree of protein binding, as a pharmacodynamic interaction may occur.
As a result of this interaction, the free fraction of escitalopram can increase and, consequently, the effects, as it’s the proportion that’s not bound to proteins that performs the action. By increasing the effects so much, toxicity could occur.
Metabolism
Metabolism or biotransformation is understood to be all the chemical reactions that occur in the body on the drug in order to make it more soluble in water and, thus, favor its elimination.
In this regard, escitalopram is metabolized in the liver, producing two metabolites, which are the molecules resulting from the chemical reactions of metabolism. Neither molecule is pharmacologically active.
The liver isoenzyme that’s primarily responsible for the metabolism of this antidepressant is CYP 2C19, although CYP 3A4 and CYP 2D6 have also been implicated.
Elimination
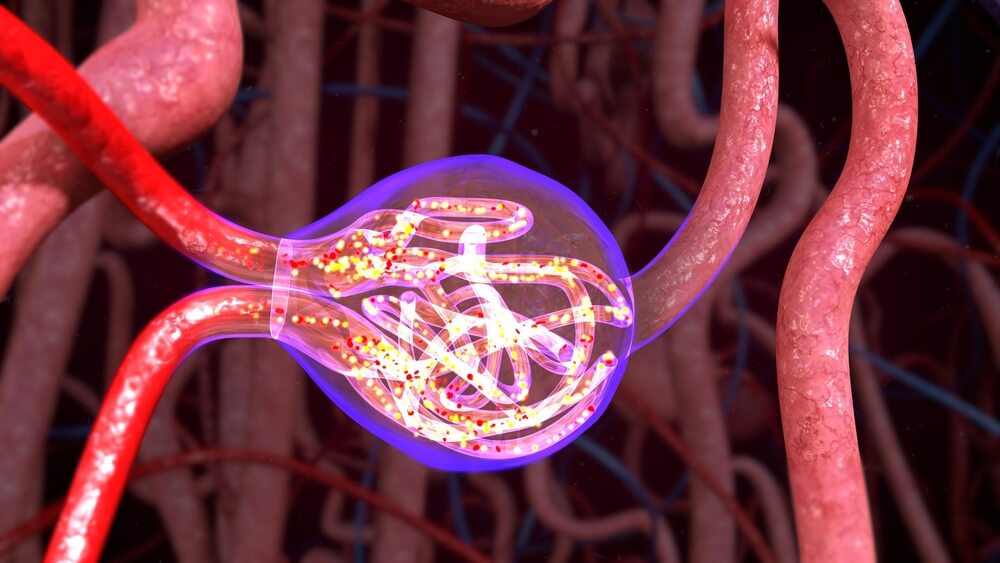
The elimination half-life after multiple doses is 30 hours, which means that this time is needed to eliminate half the concentration of escitalopram from the blood.
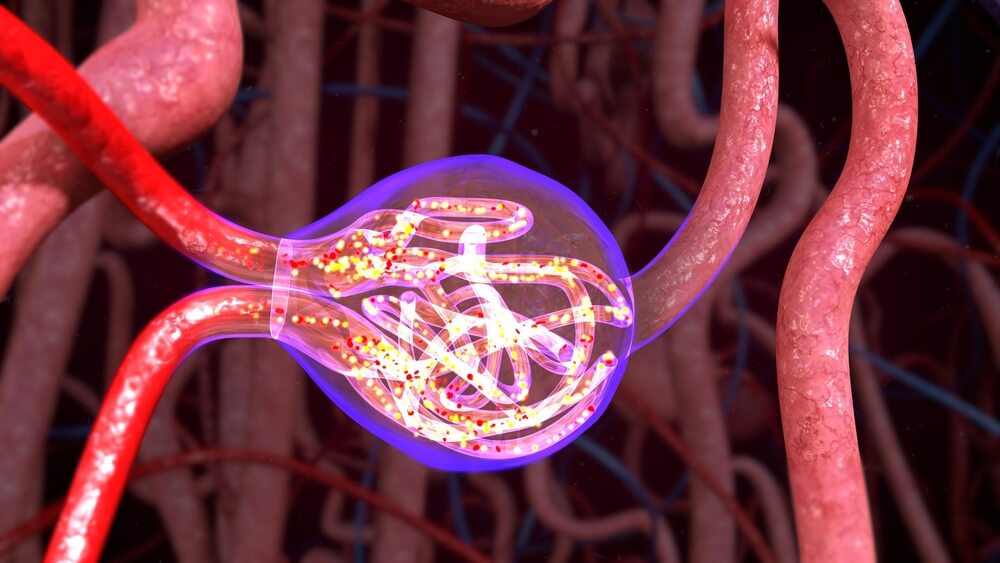
Both the molecule of origin and its metabolites are eliminated via the liver and the kidneys. Therefore, most of the dose is excreted as metabolites in the urine.
Indications and dosage
The main indication for escitalopram is depression. The usual dose is 10 mg per day, although it can be increased to a maximum of 20 mg, depending on the individual response of the patient and, obviously, as long as the doctor prescribes it.
Generally, the antidepressant effect is obtained between 2 and 4 weeks of treatment. In addition, the treatment of depressive episodes requires an initial treatment and a maintenance treatment of at least 6 months to consolidate the response.
Apart from depression, it’s also used to treat anxiety spectrum disorders such as:
- Panic disorders (panic attacks): Starting treatment with a single dose of 5 mg daily for the first week is recommended, before increasing the dose to 10 mg.
- Generalized anxiety disorder: The usual dose is 10 mg a day. As in the previous cases, it can be increased to a maximum of 20 mg, depending on the patient’s response. In addition, treatment should continue for at least 12 months. Long-term treatment for 6 months prevents relapses.
- Social phobia: The usual dose is also 10 mg per day and can also be increased up to 20 mg. Relief symptoms are usually seen within 2-4 weeks of treatment. Treatment should continue for at least 12 weeks.
- Obsessive-compulsive disorder (OCD): The dosage is the same as for other disorders. As it’s a chronic disease, patients must be treated for a sufficient period of time to ensure the absence of symptoms.
- Premenstrual dysphoric syndrome.
- Post-traumatic stress disorder.
There are a number of special populations that would still need to do a dose adjustment. These are:
- Elderly patients
- Children and adolescents
- Patients with kidney or liver failure
- Poor metabolizers of CYP 2C19
- Discontinuation of treatment
Find out: Childhood Anxiety: Symptoms, Causes, and Treatments
Adverse reactions and contraindications

Escitalopram can’t be administered in patients who are allergic to the drug or to any component of its composition. Nor can it be taken if there’s concomitant treatment with MAO inhibitors or pimozide.
At the same time, the most common side effects of treatment with this drug are:
- Headache
- Nausea
- Diarrhea
- Insomnia
Other less common side effects are anxiety, dizziness, fatigue, drowsiness, and gas, among others. In turn, some sexual dysfunctions may also appear as a result of treatments with both escitalopram and other serotonin reuptake inhibitor drugs, especially:
- Decreased desire
- Genital anesthesia
- Arousal disorders
- Delayed ejaculation
- Anorgasmia
Lastly, there are certain serious adverse reactions with which more caution must be exercised. However, they’re the least frequent.
This means that they’ve been observed in a proportion of less than 1% during the development of the drug (clinical trials in phases I, II, and III) and during its approval and commercialization (phase IV).
In fact, in this last stage, adverse reactions can be observed with a frequency lower than 0.1%. These include seizures, shortness of breath, and rhythm disturbances.
Escitalopram is a drug that has antidepressant properties. Therefore, it’s indicated in the treatment of depression and is a serotonin reuptake inhibitor, meaning it’s related to other drugs in this group with which it shares many characteristics. Some examples of these are fluoxetine and paroxetine.
Escitalopram was developed jointly by Lundbeck and Forest laboratories. Its development began in the summer of 1997, achieving its preparation and application for approval by the US FDA in March 2001.
The short development period can be attributed to the extensive experience of Lundbeck and Forest in the development of another drug with similar pharmacological properties, citalopram.
At the same time, escitalopram is the S enantiomer of citalopram, hence its rapid development. Enantiomers are a class of molecules in which in the pair of compounds, the molecule of one is a mirror image of the molecule of the other and they’re not superimposable.
Throughout the article, we’ll talk about the following aspects related to escitalopram:
- What is depression? What about serotonin?
- The mechanism of action.
- Pharmacokinetics.
- Indications and dosage.
- Adverse reactions and contraindications.
What is depression? What about serotonin?
As we’ve mentioned, escitalopram is used mainly for the treatment of depression by inhibiting the reuptake of serotonin. However, if we don’t understand these two terms well, we won’t be able to understand how this drug works.
Therefore, depression is a severe clinical illness with constant states of sadness. However, it goes further. It’s a disorder of the brain and there are many causes of its development, including genetic, biological, environmental, and psychological factors.

Among the biological factors, we can highlight that depression is associated with a deficit of the neurotransmitter serotonin. This chemical is made by the body and transmits signals between nerves, which is why it’s a neurotransmitter.
Serotonin is considered by some researchers to be the chemical responsible for maintaining the balance of our mood. Therefore, a deficit of serotonin leads to depressive states.
The mechanism of action of escitalopram
As we already know, it’s a serotonin reuptake inhibitor. Furthermore, it’s highly selective with minimal effects on the reuptake of norepinephrine and dopamine, two other neurotransmitters.
In other words, serotonin, like other neurotransmitters, is secreted by one neuron to bind with receptors on the membrane of another neighboring neuron and trigger an effect.
Later, it’s released from this receptor and some molecules return to the neuron that previously secreted it through a reuptake process.
It’s in this process where escitalopram acts, which inhibits it. By inhibiting it, the reuptake process of serotonin doesn’t take place and its concentration increases in the space between one neuron and another known as the presynaptic space. As there’s more serotonin, it can reattach to receptors on the neuron’s membrane and trigger more effect.
Escitalopram is at least 100 times more potent than the R enantiomer as a serotonin reuptake inhibitor and as an inhibitor of neuronal serotonin transport.
In addition, it has a low, almost zero, affinity for other types of biological amine receptors, which would explain why it has fewer adverse effects than other serotonin reuptake inhibitor drugs. This process is the only probable mechanism of action that explains the pharmacological and clinical effects of escitalopram.
Escitalopram pharmacokinetics
Within pharmacokinetics, which are the different processes and changes that the drug undergoes in the body, to put it in a simplified way, we’ll see the following aspects: Absorption, distribution, metabolism, and elimination.
Absorption
When the drug is administered orally, absorption is almost complete. Also, it doesn’t vary with food intake. Bioavailability, which is the actual concentration of the drug that will trigger the effect, is around 80%.
You may be interested: The Role of Serotonin in Depression
Distribution
This drug is distributed throughout the body, bound to plasma proteins in a percentage lower than 80%. This information is important to take into account if you’re taking another drug with a high degree of protein binding, as a pharmacodynamic interaction may occur.
As a result of this interaction, the free fraction of escitalopram can increase and, consequently, the effects, as it’s the proportion that’s not bound to proteins that performs the action. By increasing the effects so much, toxicity could occur.
Metabolism
Metabolism or biotransformation is understood to be all the chemical reactions that occur in the body on the drug in order to make it more soluble in water and, thus, favor its elimination.
In this regard, escitalopram is metabolized in the liver, producing two metabolites, which are the molecules resulting from the chemical reactions of metabolism. Neither molecule is pharmacologically active.
The liver isoenzyme that’s primarily responsible for the metabolism of this antidepressant is CYP 2C19, although CYP 3A4 and CYP 2D6 have also been implicated.
Elimination
The elimination half-life after multiple doses is 30 hours, which means that this time is needed to eliminate half the concentration of escitalopram from the blood.
Both the molecule of origin and its metabolites are eliminated via the liver and the kidneys. Therefore, most of the dose is excreted as metabolites in the urine.
Indications and dosage
The main indication for escitalopram is depression. The usual dose is 10 mg per day, although it can be increased to a maximum of 20 mg, depending on the individual response of the patient and, obviously, as long as the doctor prescribes it.
Generally, the antidepressant effect is obtained between 2 and 4 weeks of treatment. In addition, the treatment of depressive episodes requires an initial treatment and a maintenance treatment of at least 6 months to consolidate the response.
Apart from depression, it’s also used to treat anxiety spectrum disorders such as:
- Panic disorders (panic attacks): Starting treatment with a single dose of 5 mg daily for the first week is recommended, before increasing the dose to 10 mg.
- Generalized anxiety disorder: The usual dose is 10 mg a day. As in the previous cases, it can be increased to a maximum of 20 mg, depending on the patient’s response. In addition, treatment should continue for at least 12 months. Long-term treatment for 6 months prevents relapses.
- Social phobia: The usual dose is also 10 mg per day and can also be increased up to 20 mg. Relief symptoms are usually seen within 2-4 weeks of treatment. Treatment should continue for at least 12 weeks.
- Obsessive-compulsive disorder (OCD): The dosage is the same as for other disorders. As it’s a chronic disease, patients must be treated for a sufficient period of time to ensure the absence of symptoms.
- Premenstrual dysphoric syndrome.
- Post-traumatic stress disorder.
There are a number of special populations that would still need to do a dose adjustment. These are:
- Elderly patients
- Children and adolescents
- Patients with kidney or liver failure
- Poor metabolizers of CYP 2C19
- Discontinuation of treatment
Find out: Childhood Anxiety: Symptoms, Causes, and Treatments
Adverse reactions and contraindications

Escitalopram can’t be administered in patients who are allergic to the drug or to any component of its composition. Nor can it be taken if there’s concomitant treatment with MAO inhibitors or pimozide.
At the same time, the most common side effects of treatment with this drug are:
- Headache
- Nausea
- Diarrhea
- Insomnia
Other less common side effects are anxiety, dizziness, fatigue, drowsiness, and gas, among others. In turn, some sexual dysfunctions may also appear as a result of treatments with both escitalopram and other serotonin reuptake inhibitor drugs, especially:
- Decreased desire
- Genital anesthesia
- Arousal disorders
- Delayed ejaculation
- Anorgasmia
Lastly, there are certain serious adverse reactions with which more caution must be exercised. However, they’re the least frequent.
This means that they’ve been observed in a proportion of less than 1% during the development of the drug (clinical trials in phases I, II, and III) and during its approval and commercialization (phase IV).
In fact, in this last stage, adverse reactions can be observed with a frequency lower than 0.1%. These include seizures, shortness of breath, and rhythm disturbances.
- Sánchez, C., Bergqvist, P. B. F., Brennum, L. T., Gupta, S., Hogg, S., Larsen, A., & Wiborg, O. (2003). Escitalopram, the S-(+)-enantiomer of citalopram, is a selective serotonin reuptake inhibitor with potent effects in animal models predictive of antidepressant and anxiolytic activities. Psychopharmacology. https://doi.org/10.1007/s00213-002-1364-z
- Baldwin, D. S., Reines, E. H., Guiton, C., & Weiller, E. (2007). Escitalopram therapy for major depression and anxiety disorders. Annals of Pharmacotherapy. https://doi.org/10.1345/aph.1K089
- Owens, M. J., Knight, D. L., & Nemeroff, C. B. (2001). Second-generation SSRIs: Human monoamine transporter binding profile of escitalopram and R-fluoxetine. Biological Psychiatry. https://doi.org/10.1016/S0006-3223(01)01145-3
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.