What Is Cirrhosis?
Cirrhosis can be defined as the presence of deep and extensive scarring in the liver that disorganizes the structure of the liver tissue. Ultimately, this disorganization manifests as changes in the associated functions of the hepatocytes (affected cells).
Scars are made up of fibrous tissue that separates the tissue into nodules, one might say. This nodularity is sometimes even palpable from the outside in severe cases with a significant increase in the size of the organ.
The disease goes through stages, reaching a terminal state, if the appropriate therapeutic measures aren’t applied. In any case, hepatocytes have a high capacity for regeneration, which allows certain patients to have remarkable survival if they change their habits and undergo the appropriate procedures.
What is the liver for?
Understanding the functioning of the liver allows us to understand the symptoms that cirrhosis will have. As we’ve said, the alteration of the structure of the organ manifests itself with signs of altered metabolism.
One of the main features of the liver is the production of bile. This substance is an emulsifier for fats and fat-soluble vitamins. When poured into the small intestine, it helps in the digestion of nutrients, so the liver is assumed to be a digestive gland.
On the other hand, the organ acts as a reservoir for substances that the body may need in the future. Its storage properties are associated with carbohydrates, above all. In times of high intake, they accumulate in order to be administered when energy requirements are accelerated.
The detox function is key. The liver receives a large amount of blood and rids it of toxins and pathological foreign bodies. From a filter for microorganisms to the processing of drugs, this tissue is essential so that the blood doesn’t carry toxic substances from one place to the other.

The causes of cirrhosis
Cirrhosis is a disorder with many causes. Alcoholism is one of the addictions most linked to this disease and its approach is complicated because we’re dealing with people who don’t tend to recognize the problem in order to suspend the intake of the toxin. The situation is different with infectious causes.
Among viruses, we must mention the hepatitis viruses, especially those of type B and C. The latter has a high prevalence in certain world populations that are exposed to a kind of persistent endemic, with no decrease in the number of cases. Chronic hepatitis C infection leads to liver cancer and cirrhosis, so its severity becomes evident years after infection.
In the case of alcoholism, we must also assume that exposure to the substance creates problems due to its persistence over the years. In general, more than a decade of abuse is required to completely disrupt hepatocytes and generate fibrous scars.
Hepatitis B is a cause, but less frequent. There have been, in proportion, greater evolutions toward cirrhosis when hepatitis D infection is added. This is a delta virus that needs the B form to stay in the human body.
Less common causes of cirrhosis
A number of autoimmune disorders can cause cirrhosis as a symptom or as its own entity. They’re rarer and less frequent, but they carry serious symptoms. Such is the case of autoimmune hepatitis of genetic origin and primary biliary cirrhosis, which consists of a disorganized attack on the internal bile ducts of the liver.
As for toxic substances, besides alcohol, we must mention drugs. There are medications that have cirrhosis as a side effect if they’re administered in inadequate doses or for prolonged periods. Paracetamol, for example, a widespread analgesic and fever reducer, requires control in this regard.
Accumulations of natural substances that, in excess, lodge in the liver, damaging it, are also toxic. In hemochromatosis, for example, iron can’t be removed from the body and resides in liver cells.
The pathophysiology of cirrhosis
We talk about pathophysiology when we want to explain how a person gets sick. In this case, for cirrhosis, we want to look at the process by which the liver disorganizes and ends up altering its functions. It’s not something that happens overnight, as it takes years of progression.
Cirrhosis causes damage to liver cells, forcing them to die, regenerate improperly, or reorganize in different sites. This is accompanied by the formation of abnormal fibrous tissue that takes up space and separates the liver into nodules, making it harder.
In short, disorganization is an inappropriate response to the harm received. Always under the pretext of sustaining functionality, the organ seeks to adapt. And we’ve already said that hepatocytes have a high power of regeneration, although sometimes this is insufficient if the cause is maintained over the years.
With disorganized tissue, blood circulation in the liver is disturbed. The portal system is that which collects venous blood from the lower limbs and abdomen and takes it to the liver tissue for filtering. By not being able to cross it smoothly, this sector increases its internal pressure. This is known as portal hypertension.
If obstruction continues, then more and more back the increased pressure is shown. The portal system diverts its stagnant blood to the legs, esophagus, and abdomen. Varicose veins appear in the lower limbs, in the digestive system, and fluid accumulated in the abdominal cavity (known as ascites).
The disordered tissue doesn’t fulfill its metabolic functions. Energy reserves aren’t accumulated because there’s no space, bile isn’t poured into the intestine, and no coagulation factors are produced.
Symptoms of the disorder
The signs and symptoms of cirrhosis are explained by the change in the physiology of the organ. By not being able to filter the blood or produce the necessary metabolic substances, nor pour bile into the intestine, the alterations will come from these defects.
Among the most relevant, we’ll mention the following:
- Bleeding and hemorrhages: The lack of platelets derived from cirrhosis will prevent small wounds from being sealed in time, leading to petechiae and bruising under the skin or inside the organs.
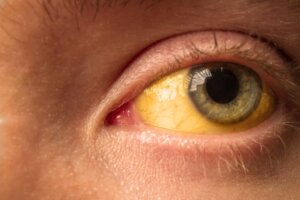
- Jaundice: This is the yellowing of the skin and mucous membranes due to the accumulation of bilirubin. As it can’t be metabolized in the hepatocytes or expelled through the bile as it should, the chemical substance adheres to other cells, causing a color change that becomes noticeable.
- Itching: Bilirubin in the skin also causes extreme itching that’s not relieved by any antihistamine.
- Ascites: This is the accumulation of fluid within the abdomen, which is expressed by an increase in abdominal body circumference and pressure on other organs in the area.
- Edema: Along with ascites, edema is fluid retention in the lower limbs, especially. Due to portal hypertension, venous blood is retained in the lower half of the body without being able to advance or reach the heart for normal circulatory exchange.
- Esophageal varicose veins: The same portal hypertension increases the caliber of the esophageal veins, which brings with it a serious complication such as upper gastrointestinal bleeding. Varicose veins rupture and cause intense life-threatening bleeding that comes out in the form of vomiting.
Ways to Diagnose Cirrhosis
The diagnosis of cirrhosis is suspected in people who accumulate a series of suggestive symptoms and who also have some risk factor. An alcoholic patient with jaundice, for example, has a high chance of suffering from the disorder.
Once the possibility is established, in addition to the physical examination, general laboratory studies that include liver enzymes are requested. Serology for viral hepatitis can be traced or antibody levels suggestive of autoimmune disease can be measured. It all depends on the suspicion.
Some signs detected in blood laboratories are indirect. That is, a record of anemia isn’t inherent to cirrhosis, but accompanies the liver problem. In the same way, low albumin concentrations aren’t only due to liver failure, but in a context such as the one we’re reporting, they contribute to characterizing the condition.
Endoscopy is a useful method for tracking esophageal varicose veins. It’s also therapeutic, as it’s possible to proceed to an elastic ligation of the veins with the same equipment.
Liver imaging is essential to establish the evolutionary degree of cirrhosis. Ultrasound, MRI, and computed tomography are used. The disorganization of the tissue is visible by these methods and, in advanced cases, there’s usually no doubt of its presence.
Finally, the option of a liver biopsy is subject to the general condition of the patient. Given the danger of excessive bleeding, it’s preferable to avoid it, although, in stabilized patients, it’s a way to certify the diagnosis.

Treatments and therapeutic options
Treatment of cirrhosis involves the use of multiple drugs to correct deficiencies and abnormal functioning. Not all patients should receive all the available pharmacology, but rather, it should be adapted to the clinical picture of each individual.
Among the options for portal hypertension, it’s addressed with beta-blockers or nitrate-type vasodilators that favor pressure reduction and adequate venous blood circulation. If there are esophageal varicose veins, it’s preferable to close them with bands designed for this purpose by endoscopy.
Hemodialysis is necessary in cases of hepatorenal syndromes. This happens when the kidney stops filtering the same way the liver did before. In conjunction, the accumulation of toxins is excessive and an artificial method is needed to supplant that lack of filtering.
Liver transplantation is the last option when support measures fail. Each country has its procedures for entering the waiting lists for organs, which will vary according to current local legislation.
Many cases of cirrhosis are preventable
Cirrhosis is preventable when its origin is in alcohol, for example. Similarly, hepatitis B can be prevented through vaccination and safe practices that prevent sexually transmitted infections. At the same time, hepatitis C is also controlled with preventive measures to control blood transfusions and reduce harm among intravenous drug users.
Liver transplantation has been an enormous advance in the survival of these patients. Its availability is increasing, but it continues to be reserved for cases of low response to conventional treatment.
Cirrhosis can be defined as the presence of deep and extensive scarring in the liver that disorganizes the structure of the liver tissue. Ultimately, this disorganization manifests as changes in the associated functions of the hepatocytes (affected cells).
Scars are made up of fibrous tissue that separates the tissue into nodules, one might say. This nodularity is sometimes even palpable from the outside in severe cases with a significant increase in the size of the organ.
The disease goes through stages, reaching a terminal state, if the appropriate therapeutic measures aren’t applied. In any case, hepatocytes have a high capacity for regeneration, which allows certain patients to have remarkable survival if they change their habits and undergo the appropriate procedures.
What is the liver for?
Understanding the functioning of the liver allows us to understand the symptoms that cirrhosis will have. As we’ve said, the alteration of the structure of the organ manifests itself with signs of altered metabolism.
One of the main features of the liver is the production of bile. This substance is an emulsifier for fats and fat-soluble vitamins. When poured into the small intestine, it helps in the digestion of nutrients, so the liver is assumed to be a digestive gland.
On the other hand, the organ acts as a reservoir for substances that the body may need in the future. Its storage properties are associated with carbohydrates, above all. In times of high intake, they accumulate in order to be administered when energy requirements are accelerated.
The detox function is key. The liver receives a large amount of blood and rids it of toxins and pathological foreign bodies. From a filter for microorganisms to the processing of drugs, this tissue is essential so that the blood doesn’t carry toxic substances from one place to the other.

The causes of cirrhosis
Cirrhosis is a disorder with many causes. Alcoholism is one of the addictions most linked to this disease and its approach is complicated because we’re dealing with people who don’t tend to recognize the problem in order to suspend the intake of the toxin. The situation is different with infectious causes.
Among viruses, we must mention the hepatitis viruses, especially those of type B and C. The latter has a high prevalence in certain world populations that are exposed to a kind of persistent endemic, with no decrease in the number of cases. Chronic hepatitis C infection leads to liver cancer and cirrhosis, so its severity becomes evident years after infection.
In the case of alcoholism, we must also assume that exposure to the substance creates problems due to its persistence over the years. In general, more than a decade of abuse is required to completely disrupt hepatocytes and generate fibrous scars.
Hepatitis B is a cause, but less frequent. There have been, in proportion, greater evolutions toward cirrhosis when hepatitis D infection is added. This is a delta virus that needs the B form to stay in the human body.
Less common causes of cirrhosis
A number of autoimmune disorders can cause cirrhosis as a symptom or as its own entity. They’re rarer and less frequent, but they carry serious symptoms. Such is the case of autoimmune hepatitis of genetic origin and primary biliary cirrhosis, which consists of a disorganized attack on the internal bile ducts of the liver.
As for toxic substances, besides alcohol, we must mention drugs. There are medications that have cirrhosis as a side effect if they’re administered in inadequate doses or for prolonged periods. Paracetamol, for example, a widespread analgesic and fever reducer, requires control in this regard.
Accumulations of natural substances that, in excess, lodge in the liver, damaging it, are also toxic. In hemochromatosis, for example, iron can’t be removed from the body and resides in liver cells.
The pathophysiology of cirrhosis
We talk about pathophysiology when we want to explain how a person gets sick. In this case, for cirrhosis, we want to look at the process by which the liver disorganizes and ends up altering its functions. It’s not something that happens overnight, as it takes years of progression.
Cirrhosis causes damage to liver cells, forcing them to die, regenerate improperly, or reorganize in different sites. This is accompanied by the formation of abnormal fibrous tissue that takes up space and separates the liver into nodules, making it harder.
In short, disorganization is an inappropriate response to the harm received. Always under the pretext of sustaining functionality, the organ seeks to adapt. And we’ve already said that hepatocytes have a high power of regeneration, although sometimes this is insufficient if the cause is maintained over the years.
With disorganized tissue, blood circulation in the liver is disturbed. The portal system is that which collects venous blood from the lower limbs and abdomen and takes it to the liver tissue for filtering. By not being able to cross it smoothly, this sector increases its internal pressure. This is known as portal hypertension.
If obstruction continues, then more and more back the increased pressure is shown. The portal system diverts its stagnant blood to the legs, esophagus, and abdomen. Varicose veins appear in the lower limbs, in the digestive system, and fluid accumulated in the abdominal cavity (known as ascites).
The disordered tissue doesn’t fulfill its metabolic functions. Energy reserves aren’t accumulated because there’s no space, bile isn’t poured into the intestine, and no coagulation factors are produced.
Symptoms of the disorder
The signs and symptoms of cirrhosis are explained by the change in the physiology of the organ. By not being able to filter the blood or produce the necessary metabolic substances, nor pour bile into the intestine, the alterations will come from these defects.
Among the most relevant, we’ll mention the following:
- Bleeding and hemorrhages: The lack of platelets derived from cirrhosis will prevent small wounds from being sealed in time, leading to petechiae and bruising under the skin or inside the organs.
- Jaundice: This is the yellowing of the skin and mucous membranes due to the accumulation of bilirubin. As it can’t be metabolized in the hepatocytes or expelled through the bile as it should, the chemical substance adheres to other cells, causing a color change that becomes noticeable.
- Itching: Bilirubin in the skin also causes extreme itching that’s not relieved by any antihistamine.
- Ascites: This is the accumulation of fluid within the abdomen, which is expressed by an increase in abdominal body circumference and pressure on other organs in the area.
- Edema: Along with ascites, edema is fluid retention in the lower limbs, especially. Due to portal hypertension, venous blood is retained in the lower half of the body without being able to advance or reach the heart for normal circulatory exchange.
- Esophageal varicose veins: The same portal hypertension increases the caliber of the esophageal veins, which brings with it a serious complication such as upper gastrointestinal bleeding. Varicose veins rupture and cause intense life-threatening bleeding that comes out in the form of vomiting.
Ways to Diagnose Cirrhosis
The diagnosis of cirrhosis is suspected in people who accumulate a series of suggestive symptoms and who also have some risk factor. An alcoholic patient with jaundice, for example, has a high chance of suffering from the disorder.
Once the possibility is established, in addition to the physical examination, general laboratory studies that include liver enzymes are requested. Serology for viral hepatitis can be traced or antibody levels suggestive of autoimmune disease can be measured. It all depends on the suspicion.
Some signs detected in blood laboratories are indirect. That is, a record of anemia isn’t inherent to cirrhosis, but accompanies the liver problem. In the same way, low albumin concentrations aren’t only due to liver failure, but in a context such as the one we’re reporting, they contribute to characterizing the condition.
Endoscopy is a useful method for tracking esophageal varicose veins. It’s also therapeutic, as it’s possible to proceed to an elastic ligation of the veins with the same equipment.
Liver imaging is essential to establish the evolutionary degree of cirrhosis. Ultrasound, MRI, and computed tomography are used. The disorganization of the tissue is visible by these methods and, in advanced cases, there’s usually no doubt of its presence.
Finally, the option of a liver biopsy is subject to the general condition of the patient. Given the danger of excessive bleeding, it’s preferable to avoid it, although, in stabilized patients, it’s a way to certify the diagnosis.

Treatments and therapeutic options
Treatment of cirrhosis involves the use of multiple drugs to correct deficiencies and abnormal functioning. Not all patients should receive all the available pharmacology, but rather, it should be adapted to the clinical picture of each individual.
Among the options for portal hypertension, it’s addressed with beta-blockers or nitrate-type vasodilators that favor pressure reduction and adequate venous blood circulation. If there are esophageal varicose veins, it’s preferable to close them with bands designed for this purpose by endoscopy.
Hemodialysis is necessary in cases of hepatorenal syndromes. This happens when the kidney stops filtering the same way the liver did before. In conjunction, the accumulation of toxins is excessive and an artificial method is needed to supplant that lack of filtering.
Liver transplantation is the last option when support measures fail. Each country has its procedures for entering the waiting lists for organs, which will vary according to current local legislation.
Many cases of cirrhosis are preventable
Cirrhosis is preventable when its origin is in alcohol, for example. Similarly, hepatitis B can be prevented through vaccination and safe practices that prevent sexually transmitted infections. At the same time, hepatitis C is also controlled with preventive measures to control blood transfusions and reduce harm among intravenous drug users.
Liver transplantation has been an enormous advance in the survival of these patients. Its availability is increasing, but it continues to be reserved for cases of low response to conventional treatment.
- McCormick, P. Aiden, and Rajiv Jalan. “Hepatic cirrhosis.” Sherlock’s Diseases of the Liver and Biliary System (2018): 107-126.
- Axley, Page D., Crit Taylor Richardson, and Ashwani K. Singal. “Epidemiology of alcohol consumption and societal burden of alcoholism and alcoholic liver disease.” Clinics in Liver Disease 23.1 (2019): 39-50.
- Brancaccio, Giuseppina, et al. “Clinical outcomes in patients with hepatitis D, cirrhosis and persistent hepatitis B virus replication, and receiving long‐term tenofovir or entecavir.” Alimentary pharmacology & therapeutics 49.8 (2019): 1071-1076.
- Zubieta-Rodríguez, Rodrigo, Jaime Gómez-Correa, and Reynaldo Rodríguez-Amaya. “Cirrosis hepática por hepatitis autoinmune: Serie de casos y revisión de la literatura.” Médicas UIS 29.2 (2016): 175-182.
- Golfeyz, Shmuel, Sara Lewis, and Ilan S. Weisberg. “Hemochromatosis: pathophysiology, evaluation, and management of hepatic iron overload with a focus on MRI.” Expert review of gastroenterology & hepatology 12.8 (2018): 767-778.
- Drolz, Andreas, et al. “Coagulation parameters and major bleeding in critically ill patients with cirrhosis.” Hepatology 64.2 (2016): 556-568.
- Bustos, Daniel Mondragón. “Ictericia.” Revista Médica Sinergia 1.7 (2016): 14-18.
- Mallet, Maxime, Marika Rudler, and Dominique Thabut. “Variceal bleeding in cirrhotic patients.” Gastroenterology report 5.3 (2017): 185-192.
- Smith, Andrew, Katrina Baumgartner, and Christopher Bositis. “Cirrhosis: diagnosis and management.” American Family Physician 100.12 (2019): 759-770.
- Villajos, Luis Téllez. Efectos del bloqueo beta-adrenérgico sobre la función cardiaca, la hemodinámica sistémica y hepática y la función renal en los pacientes con cirrosis y ascitis refractoria. Diss. Universidad de Alcalá, 2020.
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.