Polycystic Ovary Syndrome: Symptoms, Causes, and Treatment

Under normal conditions, all the hormones in the body are in perfect balance, however, when it is altered, diseases can arise. One of these pathologies is polycystic ovary syndrome, which affects many women around the world.
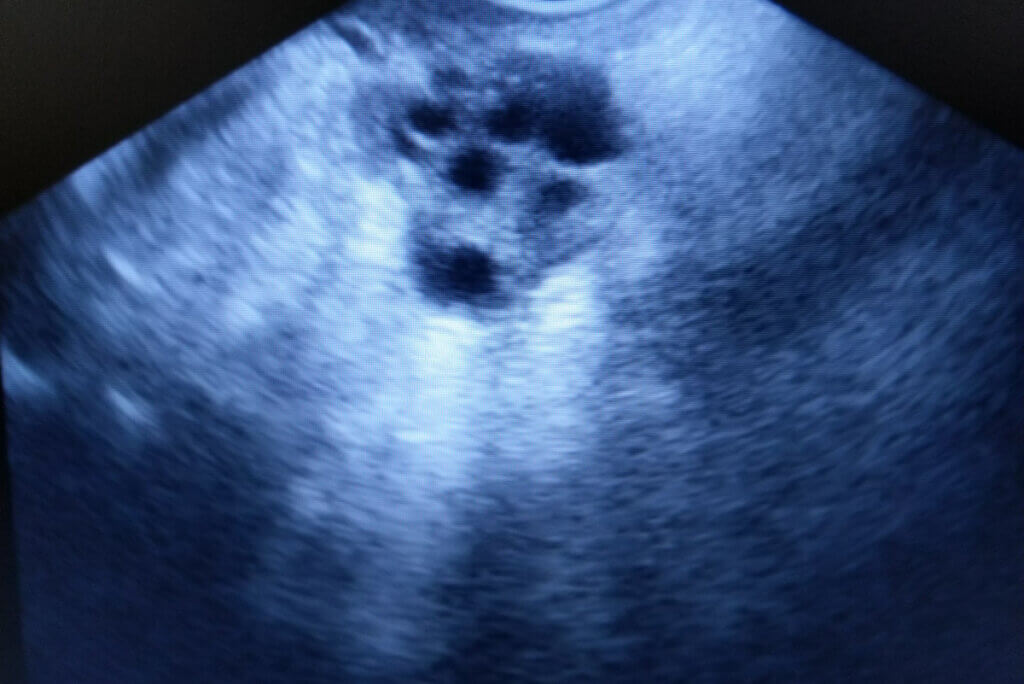
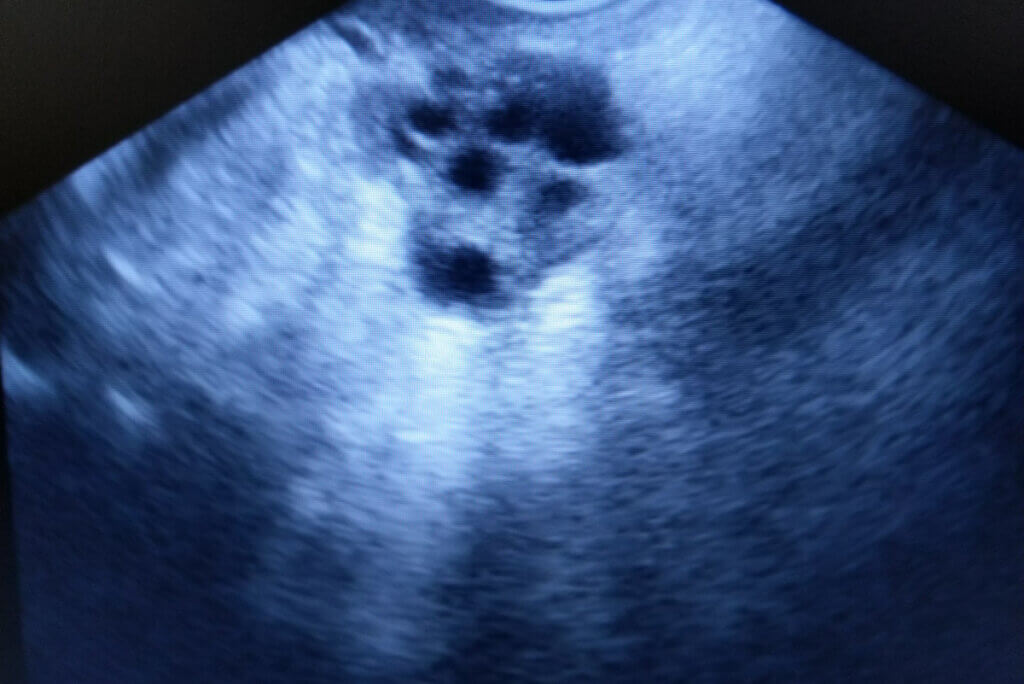
This is an endocrine disorder characterized by signs of androgen excess, mild obesity, and irregular or absent menstrual cycles. In addition, there are also various changes in the ovaries, which will have multiple follicular cysts of 2 to 6 millimeters in diameter.
Unfortunately, this is a very frequent pathology and it’s estimated that 10% of women of childbearing age suffer from it, making it the most common cause of infertility. Previously, it was believed that only fertile women could suffer from this syndrome. However, there are more and more adolescents with the characteristic symptoms.
Causes of polycystic ovary syndrome
Women synthesize progesterone, estrogens, and androgens, which are the hormones that stimulate follicular maturation and cause ovulation. In polycystic ovary syndrome there will be an excess of androgens, which will prevent the release of the mature egg, producing irregular menstrual cycles.
Sometimes, instead of forming a mature egg, the hormonal imbalance will cause the formation of ovarian cysts, which are small sacs filled with fluid. Despite being a disease discovered many years ago, doctors still don’t know the precise cause of it.
In this sense, this pathology is treated as a disease of multifactorial origin, to which heredity has been shown to be highly relevant. Recent studies discovered the role of genes involved in steroidogenesis (CYP17 and CYP11α), which regulate the expression of key hormones such as estrogen.
On the other hand, there are other factors that favor the excessive production of androgens. An example of this is excess insulin in the blood, as well as the presence of a hormone-secreting tumor.

Symptoms of the disorder
Polycystic ovary syndrome is characterized by the presence of excess weight or mild obesity, signs of hyperandrogenism, and menstrual cycle disorders, the latter being the most characteristic symptoms. In this sense, among the alterations in menstruation, the following stand out:
- Menstrual cycles longer than 45 days or as few as 9 periods per year.
- Absence of menstruation when you have already had 2 regular menstrual cycles in adolescence.
- Heavy and abnormally heavy menstrual bleeding.
- On rare occasions, absence of the first menstruation at age 16.
On the other hand, the signs of hyperandrogenism are also usually very relevant. It’s important to note that androgens are known as masculinizing hormones, so their excess in women creates physical manifestations, among we find the following:
- Abundant body hair on the face, chest, abdomen, and around the nipples.
- Acne on the face, chest or back.
- Dark, thick skin folds on the neck, groin, armpits, and breasts.
However, the appearance of male secondary sexual characteristics isn’t associated with polycystic ovary syndrome, so their appearance should be a warning indicating the presence of another disorder.
Diagnosis of polycystic ovary syndrome
Currently, there’s no specific test to diagnose PCOS. In this sense, the doctor must use the clinic and various paraclinical tests to make the confirmation.
The specialist should inquire exhaustively about menstrual changes, which are usually the main reason for consultation. However, you’ll also need to watch for abnormally distributed body hair and weight changes. Patients with the syndrome report a sudden weight change or difficulty losing weight.
In addition, a genital physical exam may be done to look for growths or lumps. Finally, an abdominal ultrasound will observe enlarged ovaries with multiple cysts.
Possible treatment
Treatment of polycystic ovary syndrome will be aimed at addressing the symptoms and complications. Thus, hormone therapy with birth control pills helps regulate menstrual cycles and can reduce signs of hyperandrogenism.
On the other hand, if you want to have children, the use of various medications that will stimulate ovulation can be recommended. Despite being possible, conception is difficult and takes a long time; therefore, one must be prudent and patient in this regard.
It’s also advisable to make a change in lifestyle and lose weight through various techniques. This simple modification increases the effectiveness of the medications, as well as helping to induce ovulation and regularize menstrual cycles.
Complications of polycystic ovarian syndrome
Excess circulating androgens and obesity affect the body. Therefore, you’ll need to see a doctor immediately if the presence of polycystic ovary syndrome is suspected. This will be the only way to have an accurate diagnosis and start treatment promptly.
When the pathology isn’t treated in time, the probability of suffering complications increases, among which we find the following:
- Arterial hypertension
- Sterility and spontaneous abortions in case of concretizing pregnancies
- Fatty liver
- Insulin resistance and type 2 diabetes mellitus
- Metabolic syndrome
- Sleep apnea
When to go and see a doctor?
It’s very important to go and see a doctor on noticing any changes in menstruation, as these are the main symptoms of the syndrome. In addition, medical attention should also be sought in the presence of any of the aforementioned signs of hyperandrogenism.
The diagnosis of polycystic ovary syndrome can affect women psychologically, due to its direct association with infertility. However, with constant medical control and the correct medication it is possible to conceive.
Under normal conditions, all the hormones in the body are in perfect balance, however, when it is altered, diseases can arise. One of these pathologies is polycystic ovary syndrome, which affects many women around the world.
This is an endocrine disorder characterized by signs of androgen excess, mild obesity, and irregular or absent menstrual cycles. In addition, there are also various changes in the ovaries, which will have multiple follicular cysts of 2 to 6 millimeters in diameter.
Unfortunately, this is a very frequent pathology and it’s estimated that 10% of women of childbearing age suffer from it, making it the most common cause of infertility. Previously, it was believed that only fertile women could suffer from this syndrome. However, there are more and more adolescents with the characteristic symptoms.
Causes of polycystic ovary syndrome
Women synthesize progesterone, estrogens, and androgens, which are the hormones that stimulate follicular maturation and cause ovulation. In polycystic ovary syndrome there will be an excess of androgens, which will prevent the release of the mature egg, producing irregular menstrual cycles.
Sometimes, instead of forming a mature egg, the hormonal imbalance will cause the formation of ovarian cysts, which are small sacs filled with fluid. Despite being a disease discovered many years ago, doctors still don’t know the precise cause of it.
In this sense, this pathology is treated as a disease of multifactorial origin, to which heredity has been shown to be highly relevant. Recent studies discovered the role of genes involved in steroidogenesis (CYP17 and CYP11α), which regulate the expression of key hormones such as estrogen.
On the other hand, there are other factors that favor the excessive production of androgens. An example of this is excess insulin in the blood, as well as the presence of a hormone-secreting tumor.

Symptoms of the disorder
Polycystic ovary syndrome is characterized by the presence of excess weight or mild obesity, signs of hyperandrogenism, and menstrual cycle disorders, the latter being the most characteristic symptoms. In this sense, among the alterations in menstruation, the following stand out:
- Menstrual cycles longer than 45 days or as few as 9 periods per year.
- Absence of menstruation when you have already had 2 regular menstrual cycles in adolescence.
- Heavy and abnormally heavy menstrual bleeding.
- On rare occasions, absence of the first menstruation at age 16.
On the other hand, the signs of hyperandrogenism are also usually very relevant. It’s important to note that androgens are known as masculinizing hormones, so their excess in women creates physical manifestations, among we find the following:
- Abundant body hair on the face, chest, abdomen, and around the nipples.
- Acne on the face, chest or back.
- Dark, thick skin folds on the neck, groin, armpits, and breasts.
However, the appearance of male secondary sexual characteristics isn’t associated with polycystic ovary syndrome, so their appearance should be a warning indicating the presence of another disorder.
Diagnosis of polycystic ovary syndrome
Currently, there’s no specific test to diagnose PCOS. In this sense, the doctor must use the clinic and various paraclinical tests to make the confirmation.
The specialist should inquire exhaustively about menstrual changes, which are usually the main reason for consultation. However, you’ll also need to watch for abnormally distributed body hair and weight changes. Patients with the syndrome report a sudden weight change or difficulty losing weight.
In addition, a genital physical exam may be done to look for growths or lumps. Finally, an abdominal ultrasound will observe enlarged ovaries with multiple cysts.
Possible treatment
Treatment of polycystic ovary syndrome will be aimed at addressing the symptoms and complications. Thus, hormone therapy with birth control pills helps regulate menstrual cycles and can reduce signs of hyperandrogenism.
On the other hand, if you want to have children, the use of various medications that will stimulate ovulation can be recommended. Despite being possible, conception is difficult and takes a long time; therefore, one must be prudent and patient in this regard.
It’s also advisable to make a change in lifestyle and lose weight through various techniques. This simple modification increases the effectiveness of the medications, as well as helping to induce ovulation and regularize menstrual cycles.
Complications of polycystic ovarian syndrome
Excess circulating androgens and obesity affect the body. Therefore, you’ll need to see a doctor immediately if the presence of polycystic ovary syndrome is suspected. This will be the only way to have an accurate diagnosis and start treatment promptly.
When the pathology isn’t treated in time, the probability of suffering complications increases, among which we find the following:
- Arterial hypertension
- Sterility and spontaneous abortions in case of concretizing pregnancies
- Fatty liver
- Insulin resistance and type 2 diabetes mellitus
- Metabolic syndrome
- Sleep apnea
When to go and see a doctor?
It’s very important to go and see a doctor on noticing any changes in menstruation, as these are the main symptoms of the syndrome. In addition, medical attention should also be sought in the presence of any of the aforementioned signs of hyperandrogenism.
The diagnosis of polycystic ovary syndrome can affect women psychologically, due to its direct association with infertility. However, with constant medical control and the correct medication it is possible to conceive.
- Ovies Carballo G, Martínez de Sandelices A, Monteagudo Peña G, Sardiñas Díaz I. Bases genéticas del síndrome de ovarios poliquísticos. Revista Cubana de Endocrinología. 2011;22(3):255-265.
- Borbón CMF, Robles QF. Síndrome de Ovario Poliquistico. Revista Clínica de la Escuela de Medicina de la Universidad de Costa Rica. 2016;6(1):134-137.
- Sir T, Preisler J, Magendzo A. Síndrome de ovario poliquístico. diagnóstico y manejo. Revista Médica Clínica Las Condes. 2013;24(5):818-826.
- De la Jara Díaz J, Ortega González C. Síndrome de ovario poliquístico. Revista Mexicana de Medicina de la Reproducción. 2011;4(2):51-62.
- Martínez L. Síndrome del ovario poliquístico [Internet]. MedlinePlus Enciclopedia Médica. 2020. Available from: https://medlineplus.gov/spanish/ency/article/000369.htm.
- Pinkerton J. Síndrome del ovario poliquístico (SOP) – Ginecología y obstetricia [Internet]. Manual MSD versión para profesionales. 2019. Available from: https://www.msdmanuals.com/es/professional/ginecolog%C3%ADa-y-obstetricia/anomal%C3%ADas-menstruales/s%C3%ADndrome-del-ovario-poliqu%C3%ADstico-sop
- Ortíz-Flores, Andrés E., Manuel Luque-Ramirez, and Héctor F. Escobar-Morreale. “Síndrome de ovario poliquístico en la mujer adulta.” Medicina Clínica 152.11 (2019): 450-457.
- Paca, Mariana Jesús Guallo. “Alimentación en adolescentes con síndrome de ovario poliquístico.” Polo del Conocimiento: Revista científico-profesional 5.7 (2020): 3-17.
- Chiliquinga Villacis, Sixto, et al. “Criterios diagnósticos y tratamiento integral terapéutico del síndrome de ovarios poliquísticos.” Revista Cubana de Obstetricia y Ginecología 43.3 (2017): 173-181.
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.