All about Hypothyroidism

To establish the presence of hypothyroidism, we must first establish that the amount of thyroid hormones present in the body is lower than normal. In this way, they’ll fail to fulfill the functions that are required for tissue metabolism.
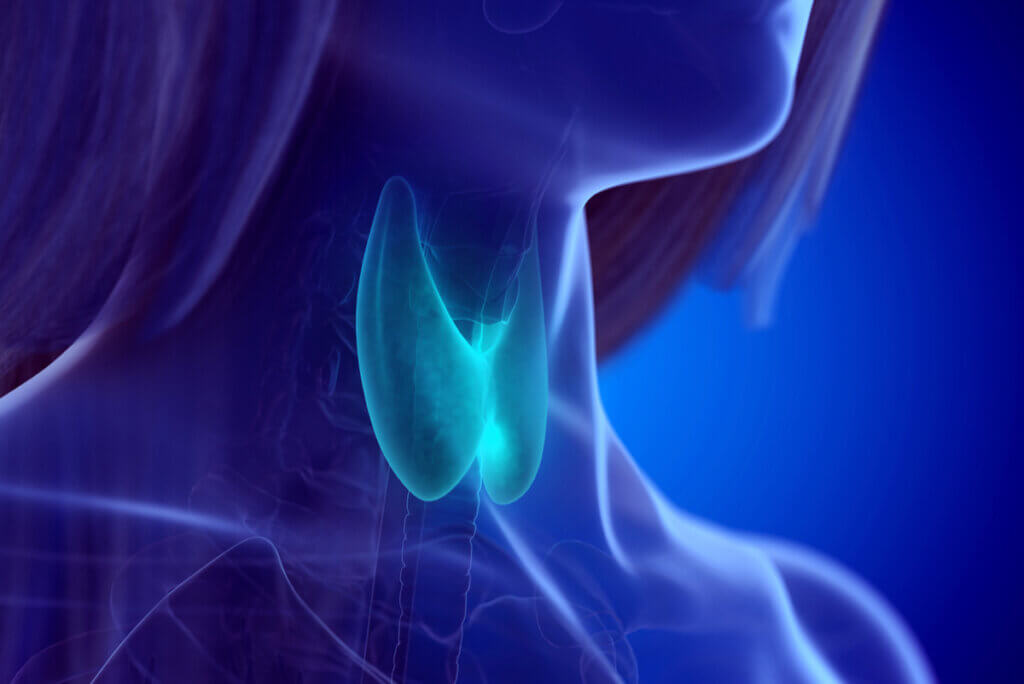
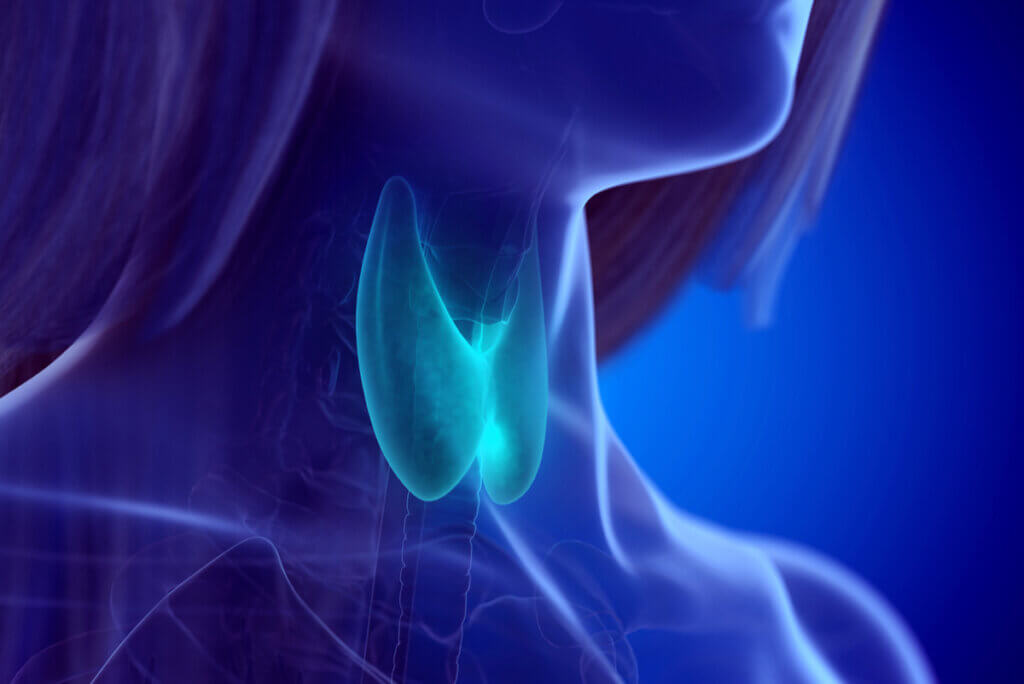
The thyroid gland, which produces these substances, is located in the neck, in the anterior part of of the neck. It’s small and consists of two lobes joined by an intermediate isthmus that isn’t usually palpable. If it becomes enlarged, it’ll then become noticeable from the outside and it can be touched with certain medical procedures.
Women are the most affected by hypothyroidism. Among them, it plays a key role in the hormonal balance that affects the menstrual cycle, since not only the sexual hormones are involved there. Moreover, it’s common for hypothyroids to have cycle disturbances among their symptoms.
Fortunately, science has discovered a way to replace the missing hormones with artificial pharmacological compounds. Levothyroxine is the drug that’s prescribed to patients to simulate this physiological action.
Causes of hypothyroidism
Hypothyroidism can be caused by other diseases that destroy the thyroid gland or by an autoimmune condition that attacks the producing cells. Either way, the end result is decreased T3 and T4 (hormones) in the blood. Unlike other disorders, there’s no cause that can be explained by their destruction once they’re already circulating.
The autoimmune form is one of the most frequent. In basic terms, the same organism recognizes the gland as foreign and begins to destroy it. The variant known as Hashimoto’s thyroiditis is the modality by which defense cells cause damage to the thyroid.
Regarding Hashimoto thyroiditis, it’s suspected that the trigger is a previous infection. In other words, the patient is affected by a bacterium or a virus that’s eliminated by the immune system, but the antibodies recognize components in the thyroid cells similar to those they attacked, so they continue their harmful action, despite the disappearance of the initial agent.
To this we must add the genetic issue. The intrinsic mechanism is also unclear, but more cases of hypothyroidism have been reported among women who have mothers, aunts, grandmothers, and sisters with the pathology. Although a specific inheritance cannot be determined, it’s clear that mechanisms linked to genes are involved.
Age also plays a fundamental role, although it isn’t a direct cause. What has been noticed is that women over 40 years of age are more likely to be hypothyroid. In part, the explanation here would be the deterioration of the gland with the aging of the metabolism. As it’s more inefficient, the production of T3 and T4 would be less.
At the same time, menopause is worth considering. As we said before, sex hormones are closely linked to the thyroid. When the last menstruation of life occurs, estrogen decreases and this alters the balance of blood substances.
The case of nodules and thyroid cancer
The presence of nodules, cysts and thyroid cancer can lead to hypo or hyperthyroidism. This is so because normal cells are replaced by non-functional or excessively functional tissue.
A large nodule or cyst is capable of eliminating part of the mechanism that produces T3 and T4. As there is less of the substance, the result is the symptoms of hypothyroidism. In cancer patients, replacement is by malignant cells that don’t have adequate functionality.
Although the most common situation is overproduction leading to hyperthyroidism, hypothyroidism shouldn’t be ruled out in these cases. These tumors tend to grow slowly, especially the papillary and follicular variants, which allows for timely detection. Not so the anaplastic form, which is 1% of all these cancers and grows rapidly.
Symptoms of hypothyroidism
The signs and symptoms of hypothyroidism are non-specific, as they can be confused with those of other pathologies and go unnoticed. However, some are almost always present, even within this variability.
It’s very rare for a patient to have acute symptoms. The usual thing is a progressiveness that occurs over the years and decades. For this reason, the diagnosis usually comes with a more established disease, although in recent times the monitoring of blood hormones has increased, which also brought about an overdiagnosis.
Among the most frequent symptoms we have the following:
- Asthenia: Tiredness and fatigue are derived from a lack of T3 and T4 that affects metabolism, especially in the muscles and brain. This will be expressed with a lack of strength and slow reactions that can cause extreme sleep. Depression has also been associated with this etiopathogenesis. Nerve transmission is slower in hypothyroidism and neurotransmitters are interrupted in their action.
- Constipation: Other things that slow down in this disease is peristalsis. The intestine is slower, so the frequency of bowel movements decreases. In part, the explanation lies in the innervation of the wall of the digestive system, which is also a victim of affected neuronal metabolism.
- Dry skin: One of the functions of thyroid hormones in the body is to maintain skin hydration through stimulation of the sweat and sebaceous glands. When it fails, the skin becomes drier and the perception of temperature is wrong. Hypothyroid patients are cold and sweat less than other people.
- Weight gain: A slow metabolism makes it difficult to assimilate nutrients, which tend to accumulate in the form of fatty tissue. This leads to an increase in body mass in the form of lipids. It isn’t always an obvious sign nor is it present in all women with the disorder, although it can result in a secondary cause of unexplained overweight.
Cardiovascular risk and hypothyroidism
A slow metabolism also affects the heart. The heart muscle works less efficiently in these circumstances and the heart rate slows. A thyroid bradycardia could then appear that may be dangerous in cases of already established arrhythmias or in the face of more demanding requirements, such as exercise.
Scientific studies have linked the lack of thyroid hormones to an increase in circulating cholesterol levels. This manifests as an increase in cardiovascular risk, since atheromatous plaques block the passage of blood in the arteries with an increased possibility of clots and thrombi.
Menstrual cycle and hypothyroidism
We have mentioned the link between hypothyroidism and menstrual cycles. This is explained by the interaction of hormones throughout the month and even once menopause has set in.
Hypothyroid women have more difficulties getting pregnant and have a higher frequency of cycle changes. They may bleed late, have heavy bleeding, or have their periods too far apart in a condition known as secondary amenorrhea.
How is hypothyroidism diagnosed?
The diagnosis of hypothyroidism is made with a blood test that checks the levels of hormones in the circulation. It’s usually requested by doctors when the presence of the disease is suspected due to obvious symptoms or the combination of several of them at the same time.
In summary, what doctors measure is the hormone TSH (thyrotropin or thyroid-stimulating hormone) and free T4 (active thyroid hormone not bound to a protein). According to the protocol used, the order of requests may vary. While some suggest measuring just TSH and then adding T4 if necessary, others advocate measuring everything in the same extraction.
TSH is included because it’s the substance that’s produced in the pituitary gland and tells the thyroid to make T3 and T4. It’s assumed that a low value of the latter will lead to a high value of TSH. Therefore, it’s an indirect sign of the presence of the illness.
In the classic picture of hypothyroidism, the diagnostic blood test shows a low free T4 level, accompanied by an elevated TSH. One variant is subclinical, with normal T4 but TSH above range.

Treatment of hypothyroidism
The therapeutic approach to this disease is based on pharmacology. The medication that’s prescribed is levothyroxine, which can be found on the market in different microgram presentations. They exist from pills with 25 micrograms to 175, 200, and 250 micrograms.
The dose is adjusted based on the weight of the patient, as it’s about simulating the natural action of the hormone. Therefore, the daily amount is variable over time and based on the physical activity that the person develops. The metabolism of an athlete isn’t the same as that of a sedentary office worker.
The pill should be taken in the morning, on an empty stomach, as this is the time when the natural hormone reaches peak levels in the blood, due to the circadian rhythm. It’s a chronic treatment and, although there are some cases in which it’s taken for a limited time, it’s most likely that patients will have to take the medication for life.
There are currently options being evaluated that could improve the therapeutic approach. They consist of combining levothyroxine with T3 artificially. Although it’s rather promising as regards more efficiently simulating the effect of natural hormones, it isn’t yet the first choice.
Both mild and severe
Hypothyroidism is a disease that’s usually mild. However, some more serious cases require special attention from health teams to detect complicated causes, such as thyroid cancer.
Given the existence of non-specific symptoms that aren’t explained by other diseases or disorders, it’s correct to request the TSH values in the blood and then proceed to confirm the pathology. The treatment is simple, so it makes no sense not to carry it out when the option exists.
To establish the presence of hypothyroidism, we must first establish that the amount of thyroid hormones present in the body is lower than normal. In this way, they’ll fail to fulfill the functions that are required for tissue metabolism.
The thyroid gland, which produces these substances, is located in the neck, in the anterior part of of the neck. It’s small and consists of two lobes joined by an intermediate isthmus that isn’t usually palpable. If it becomes enlarged, it’ll then become noticeable from the outside and it can be touched with certain medical procedures.
Women are the most affected by hypothyroidism. Among them, it plays a key role in the hormonal balance that affects the menstrual cycle, since not only the sexual hormones are involved there. Moreover, it’s common for hypothyroids to have cycle disturbances among their symptoms.
Fortunately, science has discovered a way to replace the missing hormones with artificial pharmacological compounds. Levothyroxine is the drug that’s prescribed to patients to simulate this physiological action.
Causes of hypothyroidism
Hypothyroidism can be caused by other diseases that destroy the thyroid gland or by an autoimmune condition that attacks the producing cells. Either way, the end result is decreased T3 and T4 (hormones) in the blood. Unlike other disorders, there’s no cause that can be explained by their destruction once they’re already circulating.
The autoimmune form is one of the most frequent. In basic terms, the same organism recognizes the gland as foreign and begins to destroy it. The variant known as Hashimoto’s thyroiditis is the modality by which defense cells cause damage to the thyroid.
Regarding Hashimoto thyroiditis, it’s suspected that the trigger is a previous infection. In other words, the patient is affected by a bacterium or a virus that’s eliminated by the immune system, but the antibodies recognize components in the thyroid cells similar to those they attacked, so they continue their harmful action, despite the disappearance of the initial agent.
To this we must add the genetic issue. The intrinsic mechanism is also unclear, but more cases of hypothyroidism have been reported among women who have mothers, aunts, grandmothers, and sisters with the pathology. Although a specific inheritance cannot be determined, it’s clear that mechanisms linked to genes are involved.
Age also plays a fundamental role, although it isn’t a direct cause. What has been noticed is that women over 40 years of age are more likely to be hypothyroid. In part, the explanation here would be the deterioration of the gland with the aging of the metabolism. As it’s more inefficient, the production of T3 and T4 would be less.
At the same time, menopause is worth considering. As we said before, sex hormones are closely linked to the thyroid. When the last menstruation of life occurs, estrogen decreases and this alters the balance of blood substances.
The case of nodules and thyroid cancer
The presence of nodules, cysts and thyroid cancer can lead to hypo or hyperthyroidism. This is so because normal cells are replaced by non-functional or excessively functional tissue.
A large nodule or cyst is capable of eliminating part of the mechanism that produces T3 and T4. As there is less of the substance, the result is the symptoms of hypothyroidism. In cancer patients, replacement is by malignant cells that don’t have adequate functionality.
Although the most common situation is overproduction leading to hyperthyroidism, hypothyroidism shouldn’t be ruled out in these cases. These tumors tend to grow slowly, especially the papillary and follicular variants, which allows for timely detection. Not so the anaplastic form, which is 1% of all these cancers and grows rapidly.
Symptoms of hypothyroidism
The signs and symptoms of hypothyroidism are non-specific, as they can be confused with those of other pathologies and go unnoticed. However, some are almost always present, even within this variability.
It’s very rare for a patient to have acute symptoms. The usual thing is a progressiveness that occurs over the years and decades. For this reason, the diagnosis usually comes with a more established disease, although in recent times the monitoring of blood hormones has increased, which also brought about an overdiagnosis.
Among the most frequent symptoms we have the following:
- Asthenia: Tiredness and fatigue are derived from a lack of T3 and T4 that affects metabolism, especially in the muscles and brain. This will be expressed with a lack of strength and slow reactions that can cause extreme sleep. Depression has also been associated with this etiopathogenesis. Nerve transmission is slower in hypothyroidism and neurotransmitters are interrupted in their action.
- Constipation: Other things that slow down in this disease is peristalsis. The intestine is slower, so the frequency of bowel movements decreases. In part, the explanation lies in the innervation of the wall of the digestive system, which is also a victim of affected neuronal metabolism.
- Dry skin: One of the functions of thyroid hormones in the body is to maintain skin hydration through stimulation of the sweat and sebaceous glands. When it fails, the skin becomes drier and the perception of temperature is wrong. Hypothyroid patients are cold and sweat less than other people.
- Weight gain: A slow metabolism makes it difficult to assimilate nutrients, which tend to accumulate in the form of fatty tissue. This leads to an increase in body mass in the form of lipids. It isn’t always an obvious sign nor is it present in all women with the disorder, although it can result in a secondary cause of unexplained overweight.
Cardiovascular risk and hypothyroidism
A slow metabolism also affects the heart. The heart muscle works less efficiently in these circumstances and the heart rate slows. A thyroid bradycardia could then appear that may be dangerous in cases of already established arrhythmias or in the face of more demanding requirements, such as exercise.
Scientific studies have linked the lack of thyroid hormones to an increase in circulating cholesterol levels. This manifests as an increase in cardiovascular risk, since atheromatous plaques block the passage of blood in the arteries with an increased possibility of clots and thrombi.
Menstrual cycle and hypothyroidism
We have mentioned the link between hypothyroidism and menstrual cycles. This is explained by the interaction of hormones throughout the month and even once menopause has set in.
Hypothyroid women have more difficulties getting pregnant and have a higher frequency of cycle changes. They may bleed late, have heavy bleeding, or have their periods too far apart in a condition known as secondary amenorrhea.
How is hypothyroidism diagnosed?
The diagnosis of hypothyroidism is made with a blood test that checks the levels of hormones in the circulation. It’s usually requested by doctors when the presence of the disease is suspected due to obvious symptoms or the combination of several of them at the same time.
In summary, what doctors measure is the hormone TSH (thyrotropin or thyroid-stimulating hormone) and free T4 (active thyroid hormone not bound to a protein). According to the protocol used, the order of requests may vary. While some suggest measuring just TSH and then adding T4 if necessary, others advocate measuring everything in the same extraction.
TSH is included because it’s the substance that’s produced in the pituitary gland and tells the thyroid to make T3 and T4. It’s assumed that a low value of the latter will lead to a high value of TSH. Therefore, it’s an indirect sign of the presence of the illness.
In the classic picture of hypothyroidism, the diagnostic blood test shows a low free T4 level, accompanied by an elevated TSH. One variant is subclinical, with normal T4 but TSH above range.

Treatment of hypothyroidism
The therapeutic approach to this disease is based on pharmacology. The medication that’s prescribed is levothyroxine, which can be found on the market in different microgram presentations. They exist from pills with 25 micrograms to 175, 200, and 250 micrograms.
The dose is adjusted based on the weight of the patient, as it’s about simulating the natural action of the hormone. Therefore, the daily amount is variable over time and based on the physical activity that the person develops. The metabolism of an athlete isn’t the same as that of a sedentary office worker.
The pill should be taken in the morning, on an empty stomach, as this is the time when the natural hormone reaches peak levels in the blood, due to the circadian rhythm. It’s a chronic treatment and, although there are some cases in which it’s taken for a limited time, it’s most likely that patients will have to take the medication for life.
There are currently options being evaluated that could improve the therapeutic approach. They consist of combining levothyroxine with T3 artificially. Although it’s rather promising as regards more efficiently simulating the effect of natural hormones, it isn’t yet the first choice.
Both mild and severe
Hypothyroidism is a disease that’s usually mild. However, some more serious cases require special attention from health teams to detect complicated causes, such as thyroid cancer.
Given the existence of non-specific symptoms that aren’t explained by other diseases or disorders, it’s correct to request the TSH values in the blood and then proceed to confirm the pathology. The treatment is simple, so it makes no sense not to carry it out when the option exists.
- Verdú, E. Sempere, et al. “Prevalencia del hipotiroidismo tratado en la población adulta.” Atención Primaria 35.3 (2005): 163-164.
- Hayes Dorado, Juan Pablo, and Walter Montero Justiniano. “Tiroiditis de Hashimoto en niños y adolescentes con bocio.” Revista de la Sociedad Boliviana de Pediatría 45.2 (2006): 95-97.
- Chuquimia, Génesis Astrid Marca, et al. “Perspectiva Actual del Hipotiroidismo Subclínico.” Revista SCientifica 18.1 (2020).
- de Geriatría, Sociedad Argentina, Gerontología Presidente, and José Ricardo Jauregui. “Hipotiroidismo en el anciano.”
- Mora, Angie Solano. “Nodulo tiroideo.” Revista Médica de Costa Rica y Centroamérica 73.618 (2016): 147-149.
- Cabanillas, Maria E., David G. McFadden, and Cosimo Durante. “Thyroid cancer.” The Lancet 388.10061 (2016): 2783-2795.
- Araujo, Maryory, et al. “Depresión en pacientes con hipotiroidismo y su asociación con el estado nutricional.” Revista Venezolana de Endocrinología y Metabolismo 16.2 (2018): 97-108.
- Quintanilla Ferrufino, Gustavo Jared, et al. “Alteraciones cardiovasculares causadas por hipotiroidismo clínico y subclinico.” Revista Científica Ciencia Médica 23.1 (2020): 52-60.
- Barrera, Carlos Alfonso Builes, Karen Lorena Palacios Bayona, and Fabián Alberto Jaimes Barragán. “Dosis de levotiroxina varía según la etiología del hipotiroidismo y el peso corporal.” Revista Colombiana de Endocrinología, Diabetes & Metabolismo 1.1 (2017): 27-32.
- Martín, A. Lucas. “Tratamiento del hipotiroidismo.” PATOLOGÍA TIROIDEA: 51.
- Rubio, María Antonia López, et al. “Alteración del perfil lipídico y del riesgo cardiovascular en pacientes con Hipotiroidismo subclínico.” Journal of Negative and No Positive Results: JONNPR 1.2 (2016): 45-49.
- Arauco, Ivan, Nadia Sgarbossa, and Juan Victor Ariel Franco. “Hipotiroidismo subclínico en mujeres en edad reproductiva y embarazadas.” Evidencia, actualizacion en la práctica ambulatoria 22.4 (2019): e002015-e002015.
- de la Primera Dama, Despacho. “Protocolo de atención para el diagnóstico y manejo del hipotiroidismo congénito: Actualizado julio 2020.” MSP, 2020.
Este texto se ofrece únicamente con propósitos informativos y no reemplaza la consulta con un profesional. Ante dudas, consulta a tu especialista.